Diabetes is a common and serious chronic illness among children in developed countries, but effective management can help them to lead healthy lives. Texas Children’s Hospital understands the importance of standardized, family-centered, and multidisciplinary care for patients with diabetes. To enhance diabetes care, the organization established a Clinic Care Process Team (CPT) that implemented a comprehensive approach by automating best practice alerts, enabling clinicians to identify testing needs and order labs more efficiently.
Diabetes is the most common life-threatening, chronic illness in children who live in developed countries.1 With effective management of diabetes, children with diabetes can live long, healthy, and active lives. Following evidence-based guidelines such as the routine screenings recommended by the American Diabetes Association (ADA) helps patients manage their diabetes and avoid further complications.
Texas Children’s Hospital, the nation’s largest pediatric hospital and ranked one of the top four Best Children’s Hospitals by U.S. News & World Report, believes that diabetes patients and their families are most successful in managing their disease if they receive standardized, family-centered, multidisciplinary care in both inpatient and outpatient settings. Like other leading children’s hospitals, Texas Children’s had the best intentions of adhering to the guidelines. However, team members were concerned that not all patients were receiving the ADA-recommended tests—and baseline data confirmed they were falling short. While clinicians were aware of the evidence-based guidelines, they lacked the support of data and technology that would help them keep track of every patient and their status in relation to the guidelines. Clinicians were also concerned that variation in care and gaps in communication were negatively impacting patient satisfaction and empowerment.
To tackle this multi-faceted problem, Texas Children’s created a new Clinic Care Process Team (CPT). The team developed a comprehensive approach to standardizing diabetes care by automating best practice alerts that help clinicians recognize the need for testing so they order labs more quickly. The alerts were designed to ease the burden on physicians and streamline the process. The team also listened to feedback from patients and parents to create new diabetes action plans, standard welcome letters, and brochures to ensure that patients and families receive the information they need to feel confident and informed.
These initiatives resulted in measurable improvements within one month of implementation:
Millions of children and families across America live with the challenge of managing diabetes. Texas Children’s evaluates over 2,500 pediatric diabetes cases each year. As a leader in research and treatment, the hospital’s mission is to help children, adolescents, and young adults manage their diabetes so they can live long and healthy lives. Providing standardized diabetes treatment is vital to this important mission.
The ADA’s Standards of Care provide guidance for hospitals like Texas Children’s looking to provide the best care for patients struggling with this difficult disease. The standards outline the components of effective diabetes care and treatment goals, along with the recommended guidelines for screening, diagnostic, and therapeutic actions thought to positively affect patient outcomes.2
The team at Texas Children’s Diabetes and Endocrine Care Center wanted to deliver on their mission— ensuring coordinated, family centered, multidisciplinary care that allows and empowers patients and their families to take an active, central role in their diabetes management. However, the complexity of diabetes created challenges for clinicians who had to address a lengthy list of concerns at each patient visit, leaving little time to focus on routine annual screenings and the patient experience. Despite the best intentions, team members were concerned that not all patients with type 1 and type 2 diabetes were receiving the routine screening labs. They determined that clinicians were aware of the evidence-based guidelines but found it difficult to adhere to them because patient data was not easily accessible.
Previously, busy clinicians were required to recall patients’ last dates of testing from memory or conduct a time-consuming search through the EHR. Team members needed to establish a reliable process, leveraging technology, to support clinicians in these efforts. They also determined that the patient experience could be improved—especially for new patients and families overwhelmed by a life changing diabetes diagnosis. These new patients, along with those facing the ongoing challenge of managing diabetes at home, needed to be more educated and informed with clear, consistent, and actionable instructions for their care.
Clinicians at Texas Children’s set out to develop an innovative outpatient program that would provide coordinated, family-centered, multidisciplinary care to their patients. They focused their efforts on three key initiatives:
Their first step was to establish the Clinic CPT. This physician-led improvement team is comprised of clinicians, administrative staff, dieticians, educators, social workers, medical assistants, registered nurses, and parents. Capturing the voice of the patient through parents helped the team gain a more comprehensive perspective on pain points. Parents provided valuable insights on how the team could empower patients and their families to take an active and central role in their diabetes management. By using performance data from the Health Catalyst Analytics Platform built using the Late-Binding™ Data Warehouse architecture (EDW), the Clinic CPT identified the opportunity for improvement in the adherence to ADA recommendations (see Figure 1) for annual screenings of patients with both type 1 and type 2 diabetes. The annual screening is important. There is no risk associated with the screening tests, providing only benefit to the patient. The earlier the complications of diabetes are identified, the more effectively they can be managed, lowering the risk of substantial complications and improving quality of life long term. Once baseline data confirmed that not enough patients were receiving the recommended annual screening, the Clinic CPT began to take action.
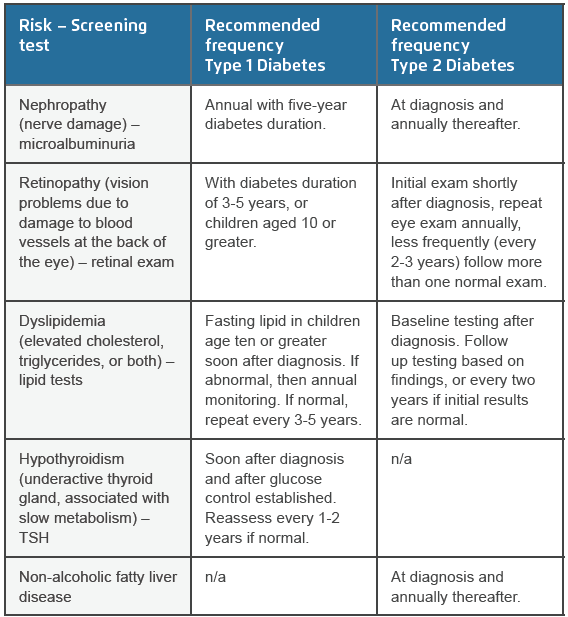
Clinic CPT members wanted to increase adherence to the ADA guidelines without increasing the burden on clinicians or patients. They chose to harness the power of technology to drive out variability, embedding decision support in the EHR to alert the clinicians of the recommended labs. The alerts, which had been successful in Texas Children’s inpatient treatment, were built to be congruent with the ADA recommendations for each screening in relation to patient age, time from diagnosis, and type of diabetes. The alerts fire during the clinic visit for patients who have not undergone the tests and clinicians can order labs in real time while resolving the alert. This one-piece workflow greatly increases the likelihood that the recommended test will be ordered and conducted in a timely manner. Team members worked directly with IT to build and test the new technology in the EHR. They also took initiative to drive adoption of the alerts by presenting information at medical staff meetings and distributing written information via email. In addition, they ensured that IT staff were available during the go-live period to provide clinician support and resolve any issues related to the alerts.
The final piece of the Clinic CPT’s strategy focused on improving patient satisfaction and confidence in the self-management of diabetes at home with better communication and education. When pediatric patients are first diagnosed with diabetes, the change can be overwhelming for parents who leave the clinic with a child whose condition is significantly more complex than when they arrived. Managing that medical complexity can be difficult for parents, especially if they do not receive clear, actionable instructions that support their ability to manage the diabetes at home. Listening to the parents’ perspectives helped the Clinic CPT to understand the gaps in communication, especially for those new patients who have been identified as high risk for complications, necessitating additional education and support.
Working closely with a Community CPT, the Clinic CPT prioritized the standardization of workflow for new patients, the development and standardization of new, color-coded diabetes action plans, and the standardization of insulin guidance forms. For new patients, the team created a standard welcome letter that outlines what to expect from the clinic and what the clinic expects from them. It sets clear expectations about the length of time patients will typically spend at each visit, and the importance of bringing their glucose meter/insulin pump and snacks to their appointment. The information explains that care will be provided by a multidisciplinary team, including social workers, diabetes educators, and dieticians with whom they will have annual visits. The purpose and importance of the visits is emphasized so patients and parents understand that these visits are designed to help them get the most out of their diabetes care.
To empower patients and parents to effectively manage the medical complexity of diabetes at home, the Clinic CPT developed standard diabetes action plans (see Figure 2). The action plans outline the steps patients and parents should take for commonly encountered problems. The best action plans include written information that is easily understood by patients, with colored zones that correspond to the level of concern (green, yellow, orange, red). Insulin dose guidance forms were also standardized to further reduce variability and guarantee that the clinic is providing care that aligns with evidence-based recommendations.
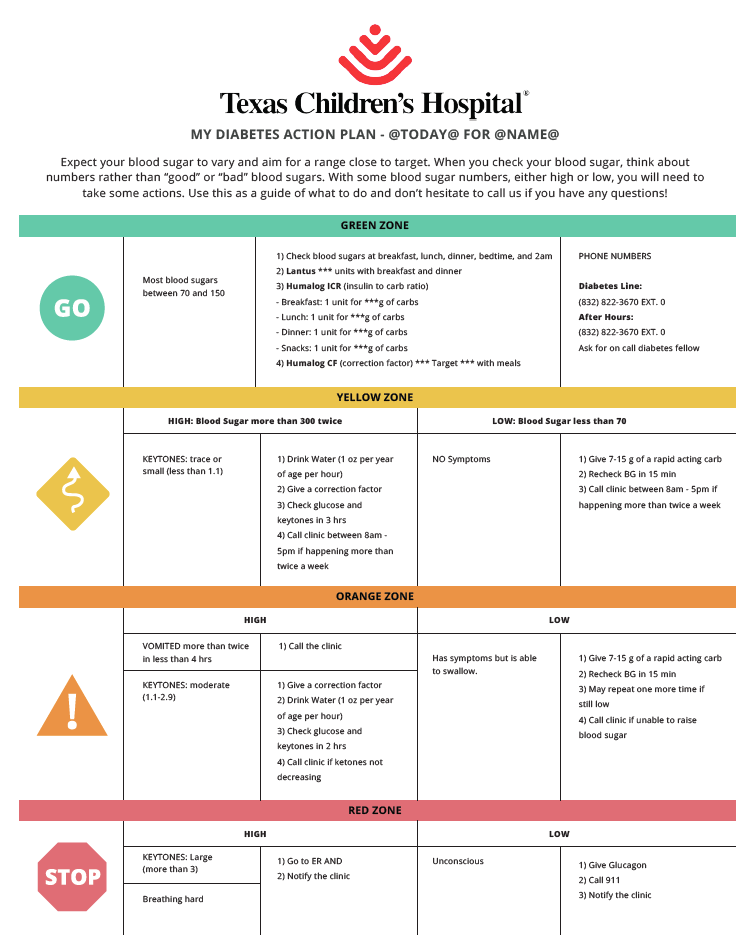
The Clinic CPT also leveraged the standard education curriculum for diabetes developed by the Education CPT. Those brief but informative brochures touch on key details such as what patients and families should expect to happen immediately related to glucose regulation; information about labs the clinic may want to check; and, how to prevent future problems. Psychologists reviewed all written materials to ensure the language used would be well received by the patients. Versions were also created in Spanish due to the large number of Spanish speaking individuals who receive care at Texas Children’s.
By standardizing clinic processes, using technology to improve reliability and monitor performance, and providing consistent messages to patients and their families, the Clinic CPT at Texas Children’s is achieving impressive results. Within one month of implementing the decision support alerts, screening percentages for each test improved to greater than 80 percent and performance has continued to advance.
The Clinic CPT wants Texas Children’s clinics to be a place that children and families are excited to visit. More importantly, the team wants patients to feel confident that they will receive the best education and highest quality care while at the clinic. Team members have identified three key action items:
“We want our patients and families to feel engaged, educated, and empowered when making decisions about their care at home. That confidence is critical to their ability to manage their diabetes, not just in the short term but also throughout their lifetime.”
– Sara Bartz, MD, Diabetes and Endocrinology