To optimize the impact of its diabetes self-management education program, Allina Health enhanced its service model, aligning resources to proactively meet patient demand, while also maintaining high-quality clinical outcomes. Utilizing analytics in the redesign process has allowed Allina Health to understand patient needs better and monitor the impact of planned changes to the program on patient outcomes.
Diabetes affects more than 30 million people in the U.S., with costs exceeding $30 billion annually, making it the most expensive chronic disease to manage in this country. Effective treatment, however, is dependent upon patient knowledge and self-management.
To optimize the impact of its diabetes self-management education program, Allina Health needed to move away from a service model that required the certified diabetic educators (CDEs) to travel to 42 different clinics and to a more effective model, aligning resources to proactively meet patient demand, while also maintaining high-quality clinical outcomes. Utilizing analytics in the redesign process has allowed Allina Health to understand patient needs better and monitor the impact of planned changes to the program on patient outcomes
Diabetes affects more than 30 million people, with successful treatment depending on proper patient self-management. It is currently the costliest chronic disease to manage in the U.S., with associated costs exceeding $30 billion annually.1
As a specialty medical service, diabetes self-management education (DSME) programs help people navigate the decisions and activities necessary for diabetes self-care through consultation, group classes, medicine management, prediabetes classes, and care for diabetes in pregnancy.2
Diabetes treatment is meant to maintain glycemic control and prevent tissue damage caused by excessive glucose in the bloodstream. Glycemic control is measured with a hemoglobin A1c (HbA1c) blood test that reflects glucose levels over the previous three months. Maintaining glycemic control is dependent upon patient knowledge, self-care, provider follow-up, and medication adjustments.3
Allina Health, a not-for-profit integrated healthcare delivery system, is dedicated to the prevention and treatment of illness, and enhancing the greater health of individuals, families, and communities throughout Minnesota and western Wisconsin. Through its 12 hospitals, 90+ clinics, 15 pharmacies, and specialty medical services, the organization cares for patients from beginning . to end-of-life. Diabetes impacts many of Allina Health’s patients, making it a priority to help them self-manage the disease.
In response to the increasing number of patients with diabetes and to maximize healthcare resources, Allina Health implemented a DSME program that was overseen by a team of CDEs, registered nurses, and registered dieticians.
Through the DSME program, individual CDEs provided services to 42 clinic locations across seven geographical regions that included an initial 60-minute visit followed by subsequent 30-minute medication management visits. CDEs traveled between multiple locations each day.
The program was initially successful. HbA1c levels decreased an average of 13.4 percent after the initial CDE visit, which represented a clinical improvement in population health, and net revenue was positive during the first year of operation. As CDE referrals increased, however, significant problems began to develop with the service model, including:
The decrease in productivity had a domino effect that impacted both patient and provider satisfaction, patient engagement, diabetic self-care clinical services, outcomes, and net revenue. Allina Health needed a DSME program service model that did not require CDEs to travel to 42 different clinics and was effective, aligning resources to proactively meet patient demand, while also maintaining high-quality clinical outcomes.
Allina Health committed to establishing a patient-centric solution for improving the DSME program’s clinical outcomes and processes. The organization elicited feedback and support from departmental, operational, and physician leaders, along with frontline clinical staff, healthcare providers, patients using DSME services, and CDE staff, asking them to partner with the organization to identify, troubleshoot, and improve DSME processes and services.
Recognizing the need to redesign the DSME workflow for better patient access, productivity, and scheduling, Allina Health chose to move away from providing service at all locations to a ‘hub’ model.
Prior to making alterations, leaders engaged with individual providers and groups, using adaptive change management strategies to discuss the need for a change in service delivery. Leaders listened to and addressed concerns, garnering support for transformation. DSME leaders then leveraged data from the EMR and the Health Catalyst® Data Operating System™ (DOS) platform and a robust set of analytics applications to better understand patient needs, and monitor the impact of planned changes on patient outcomes.
Using the diabetes program analytics application, Allina Health can evaluate and understand DSME program performance, including cost, clinical outcomes, operational effectiveness, and patient engagement (see Figure 1).

The analytics application includes a variety of filters, enabling DSME program leaders to perform in-depth analysis. Performance measures can be filtered by location, CDE, and patient demographics including ethnicity, financial class, age, gender, type 1 diabetes, type 2 diabetes, and gestational diabetes (see Figure 2).
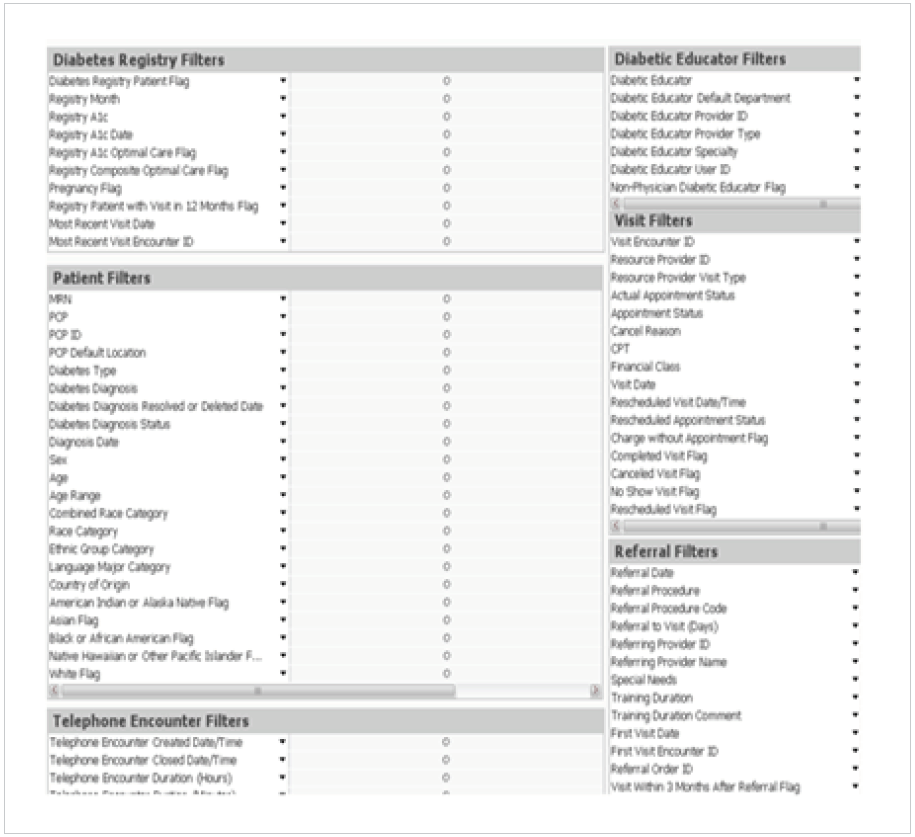
Using the analytics application, Allina Health could identify utilization of the DSME program across the 42 clinics. The organization evaluated referral volumes, geography, patient demographics, support for endocrinology, and the physical space available for patient encounters, using these data to make decisions about the number and placement of locations for its DSME services.
Ultimately, the organization selected 12 locations for DSME service, allowing CDE staff to conduct visits at the hub locations Monday through Friday. In addition to using data from the analytics application to understand patient needs and identify the best locations for the centralized hubs, Allina Health conducted a time study, identifying opportunities to streamline the processes used for documentation of visits and the processes used to conduct follow-up phone calls.
Allina Health standardized DSME visit length and streamlined documentation in the EMR. CDEs use a specific encounter form that includes preferred medications for the patient’s health plan, helping to ensure patients receive the right medication at the lowest possible cost.
Allina Health developed and embedded a documentation flowsheet within the encounter, ensuring that all content required for reimbursement is accurately documented, and improving CDE documentation efficiency. The information needed for the American Diabetes Association certification is entered in discrete fields, decreasing the manual work required for annual reporting processes.
Patient access, scheduling, and CDE productivity improved through implementing an electronic pool created to capture phone communication and ensure prompt routing to CDEs for expedited communication. Phone calls from patients, primary care providers, or endocrinologists are routed to an electronic pool where any available CDE can respond to the call, eliminating both the need for voicemail and the lag-time that had negatively impacted patient satisfaction and contributed to no-shows.
By implementing a data-driven, patient-centric model, Allina Health has increased CDE productivity, improved provider and patient utilization along with satisfaction, and expanded DSME program capacity, providing diabetes self-management services that produce high-quality clinical outcomes. Results include:
“Diabetes management is challenged by the growing population, complexity of the disease, and its treatments. This requires a unique care delivery structure and team approach.”
– Dawn McCarter, RN, BSN, CDE Manager, Diabetes Education
Allina Health will continue to improve its DSME program, using analytics to monitor its effectiveness and taking a data-driven approach to improving chronic disease management.