Texas Children’s Hospital recognized the need for effective diabetes self-management education for pediatric and adolescent patients and their families to improve clinical outcomes and quality of life. To address inconsistencies in education and the lack of organizational standards, the hospital established an Education Care Process Team (CPT). This team developed a standardized curriculum based on national guidelines, created uniform educational materials, and utilized analytics to identify learning gaps and customize patient goals.
Effectively educating pediatric and adolescent patients and families to self-manage diabetes is a critical part of diabetes care. Leaders at Texas Children’s Hospital, one of the top four children’s hospitals in the country, recognized that diabetes education that incorporates national standards and empowers patients can improve clinical outcomes and quality of life. While diabetes education has always been important to Texas Children’s, the education provided to patients was varied, no organizational standards existed, and tracking the effectiveness was not possible.
To address these challenges, Texas Children’s created an Education Care Process Team (CPT) that focused on: developing a standard education curriculum based on national guidelines, creating consistent education materials, leveraging powerful analytics to identify potential learning gaps and customize patient goals, and investing in the professionals who deliver education.
Texas Children’s Hospital, ranked as one of the top four Best Children’s Hospitals by U.S. News & World Report, is a leader in the research and treatment of children with diabetes, evaluating more than 2,500 cases annually. Whereas diseases such as hypertension or high cholesterol can often be treated with behavior modification and medication, diabetes is much more complex. Effective diabetes management requires that the patient and family understand the diabetes disease process and how to manage nutrition, physical activity, glucose monitoring, and psychosocial challenges.1
Diabetes education that incorporates national standards for diabetes self-management education (DSME) from the American Association of Diabetes Educators (AADE) and the American Diabetes Association (ADA) Task Force is an essential component of effective care.2 Patient-centered diabetes education can improve clinical outcomes and quality of life. Models of education that empower the patient and that include behavioral goal-setting are most effective.3
At Texas Children’s, diabetes education has always been a part of the care and support provided to patients and their families. The goal of diabetes education is self-management of the disease by the patient and their family. Providing education for children with diabetes poses some unique challenges. For children diagnosed at a young age, parents are often the recipients of education to help them managed their children’s diabetes. As children develop and approach adolescence, education that has previously been conveyed to the parents needs to be revisited, with the focus on the delivery of developmentally and age appropriate education for patients that allows them to effectively self-manage their diabetes. Diabetes self-management education should also include support and encouragement. Diabetes education has evolved over time, with the literature indicating that primarily didactic presentation, where the educator simply presents information to the patient, is not as effective as models that engage and empower the patient.
Texas Children’s identified that the education they provided to its patients was not as effective as it could be, for a number of reasons.
Texas Children’s knew that it needed to address these challenges in order to deliver patient-centered education that: aligned with current national recommendations, met the unique needs of their local population, and was a product of which they could be proud.
To ensure that the diabetes education provided was the quality that Texas Children’s needed, including alignment with national recommendations, Texas Children’s formed the Education Care Process Team (CPT). This team is integrated within the larger Diabetes CPT. The Education CPT is a physician-led, interdisciplinary team composed of diabetes providers, educators, psychologists, dietitians, social workers, marketing professionals, parents, and community experts in education. The Education CPT was tasked with improving the quality of the materials used in the ambulatory setting, defining and creating a standard for diabetes education at Texas Children’s, and developing changes in clinic processes to improve the patient education experience. At the time the Education CPT was developed, the diabetes educators had recently changed their team configuration and reporting relationship and were in the midst of reorganizing their educational materials. This provided an ideal opportunity for the diabetes educators to align these initiatives with the work of the Education CPT.
To get started, the team conducted an inventory of all available written education materials, resulting in a stack more than 1.5 feet tall. A preliminary review of these resources confirmed what Texas Children’s had suspected, that the materials were not consistent. While the content did touch on all of the key areas recommended by the AADE/ADA Task Force, there was no consistent approach or defined curriculum. The Education CPT embarked on a process to establish a standard curriculum for diabetes education across Texas Children’s. They began by conducting a detailed evaluation of all the educational materials, assessing the quality of the content and supporting materials, appropriateness of the delivery method (written, verbal, multimedia), and congruence with national recommendations.
Based on their assessments, the diabetes educators and Education CPT revised the written materials to ensure they were consistent with the AADE/ADA national standards for diabetes self management. Additionally, they developed educational content to meet region-specific needs, such as emergency preparedness in case of hurricanes. To ensure the revised educational materials would be well-received by patients and families, psychologists reviewed them to make sure the wording was developmentally appropriate and conveyed in a positive manner. Patients also were asked to review the materials and provide their feedback about readability and appropriateness.
The Education CPT next redesigned how the education curriculum is delivered, moving away from a traditional didactic approach to a patient-centered approach that includes assessment of individual patient and family needs, motivational interviewing to support goal setting, implementation of ongoing education and motivational support to help patients achieve those goals, and monitoring/evaluation of the patient/family’s ability to achieve their goals.
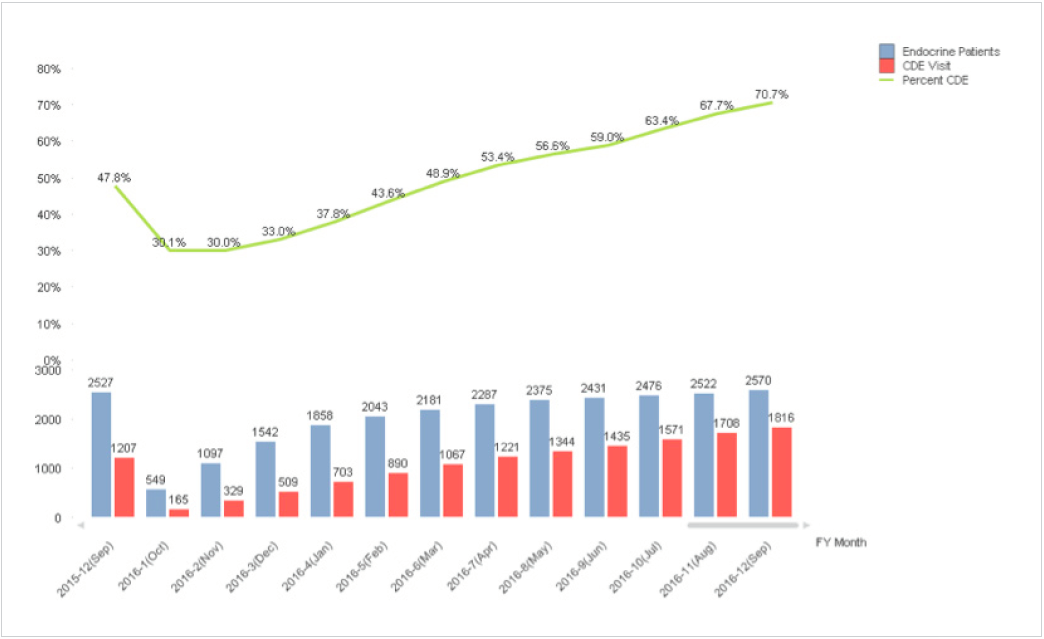
Prior to this initiative, patient education did not take place consistently. Typically, education was offered to patients in the clinic at the end of the appointment, and it was perceived to be optional. Patients/families would frequently decline, hindering the skill development required for successful diabetes self-management for many patients. In addition, patient education was not documented in a manner that supported a step-wise approach, which limited the ability of diabetes educators to build on previously provided education. As a remedy for these problems, the Education CPT developed a standard workflow to integrate diabetes education within the clinics. Now, rather than waiting until the end of the patient’s appointment to offer education, the clinic team conducts a pre-visit huddle, identifies any unique learning needs, and establishes an education plan for that visit. In addition, patients now complete a pre-visit questionnaire, which allows them to self identify the educational areas of greatest need and helps the care team plan how to best address those needs. Texas Children’s goal is for at least 80 percent of their patients to have a visit with a diabetes educator each year. To help achieve this goal, each patient is scheduled for a visit with the diabetes educator, with high-risk patients supported by the educator at every visit.
Texas Children’s has leveraged technology to improve the effectiveness of the education program, track patient education, and identify potential gaps in the patient education process. The EHR system was updated to include an education-specific flowsheet where patient education can be thoroughly documented. The team is able to review this information to build on previously delivered patient education.
Additionally, the Health Catalyst Analytics Platform built using the Late-Binding™ Data Warehouse architecture (EDW) enables further improvements to the education process. The team is able to use data from the EDW to prospectively identify potential gaps in education, and analytics allows the team to quickly visualize the number of patients who have been seen by the diabetes educator. The team is able to easily and quickly identify the patients who have not been seen for an extended period of time and can follow up with those patients. For each patient scheduled to be seen, the education team is able to use the data in the EDW to identify what the patient-specific education needs are. The team is now purposeful in using data to inform the education plan, in addition to the goals identified by the patient/family.
Texas Children’s has also placed a high priority on developing the knowledge and skills of the professionals who provide diabetes patient education. Understanding that national certification is a mark of excellence that demonstrates comprehensive knowledge and experience in diabetes management, pre-diabetes, and diabetes prevention, all educators who did not already possess credentials as certified diabetes educators (CDEs) were asked to obtain the national certification.
Leaders also took steps to build relationships with school nurses in the community. School nurses play an important role in the support of children with diabetes and may be the first to recognize potential health problems and complications associated with diabetes. They frequently assist school-age children and their families with effective disease management. To support school nurses and improve their knowledge, Texas Children’s hosted an educational conference, which more than 100 school nurses attended. During the conference, a school nurse approached one of the CDEs, talking with her about a teenage patient with whom they both worked. The teenager was on a simplified insulin management plan, and his glucose control was not optimal due to regular blood glucose highs and lows. The CDE who had been working with the patient had previously spoken with him about changing from a simplified insulin management plan to an insulin-to-carb ratio. Using the newly standardized education curriculum, the CDE was able to easily teach the teenager how to count carbs, read food labels, and then calculate the appropriate dose of insulin. The teenager was successful at better controlling his glucose, and his progress was apparent to the school nurse. The school nurse shared with the CDE feedback on the positive impact of the changes. She said the teenager always had great potential, but his high and low glucose levels were impairing his ability to effectively participate in school and learn. Since changing to the insulin-to-carb ratio, he was better able to participate in school activities and was getting better grades. This was just one of many patient success stories that has occurred as a result of Texas Children’s renewed focus on consistent, well-executed, patient-centered diabetes education.
The Education CPT has achieved their team goals, including:
“Using analytics, we are able to identify patients who are not yet using an insulin pump. Rather than waiting until a patient is on an insulin pump to provide education, we can now provide education to potential pump candidates to support their decision-making process, increasing readiness for self-management.”
– Sarah Lyons, MD, Endocrinologist
Now that standard diabetes education curriculum is in place, Texas Children’s plans to embark on the next step of their educational journey, evaluating education delivery methods that better engage pediatric patients and their families to develop the skills required for effective self-management. They are exploring opportunities to increase the use of on-demand education, including games, videos and interactive applications, including more interactive, hands-on classroom opportunities.