Mission Health sought to enhance clinical outcomes for bowel surgery patients by implementing evidence-based care process models (CPMs). Its initiatives aimed to reduce length of stay, readmissions, and surgical site infections. By using data and analytics, the organization successfully improved patient care and achieved significant advancements in bowel surgery outcomes.
The consequences of poor-quality surgical care are significant for both hospitals and patients. Consider the following: One in four patients having a colon re-section is readmitted within 90 days, costing U.S. healthcare approximately $300 million a year and negatively affecting the lives of tens of thousands of patients and their families.
In 2013, Mission Health, North Carolina’s sixth-largest health system, identified opportunities to improve clinical outcomes for its bowel surgery patients. With a vision of achieving the best outcome for each patient, Mission set goals to reduce length of stay (LOS), decrease readmissions, and reduce surgical site infections (SSIs) for its bowel surgery patients.
Mission recognized that care process models (CPMs) were key to making it easier for clinicians to deliver the best care to patients by doing the right thing consistently. The health system therefore organized a multidisciplinary improvement team charged with developing and implementing an evidence-based CPM for bowel surgery. In support of this effort, Mission leveraged technology and analytics to encourage clinician adoption of the CPM and to deliver performance insights.
Through these efforts, Mission has achieved impressive improvements in bowel surgery care.
Value-based care demands the highest-quality performance from surgeons. The consequences of poor quality are significant for both hospitals and patients.
Increasingly, hospitals are penalized for preventable complications, such as SSIs.1 Hospitals face even more costs from complications that result in readmission. The case of colon resections provides a sobering example of these readmission costs. For this type of bowel surgery, one in four patients in the United States is readmitted within 90 days, costing approximately $9,000 per patient, or $300 million a year.2
While the financial implications of surgical complications are compelling, the impact on patient experience and patient outcomes is even more concerning to health systems like Mission Health, whose aim is to achieve the optimal outcome for each patient, first without harm, also without waste, and with an exceptional experience for the patient and family.
North Carolina’s sixth-largest health system, Mission strives to provide world-class care to patients and their families when they need it most. When it identified opportunities to improve clinical outcomes clinical outcomes for its bowel surgery patients, Mission took action.
In 2013, Mission set goals to reduce LOS, decrease readmissions, and reduce SSIs for its bowel surgery patients. To accomplish these goals, Mission leaders knew they needed to identify processes and care routines that would result in the desired improvements, as well as find a way to ensure ongoing adoption of these best practices to sustain improved outcomes.
However, Mission’s bowel surgery improvement effort faced a significant barrier: To get baselines or strategic direction on the patient population required hours of data gathering and manual interpretation. The resulting lack of digestible data prevented Mission from designing comprehensive performance improvement initiatives to improve bowel surgery outcomes.
For example, due to varying complexity by case, Mission was challenged to determine how much opportunity for improvement truly existed with respect to LOS and readmission rates for bowel surgery patients. The health system needed to account for factors that varied the complexity of each case, but it lacked the data or analytics infrastructure to effectively stratify patients.
Without this ability, surgeons couldn’t see the overall or changing risk of their patient population or identify the key drivers behind outcomes. At the same time, members of the quality improvement team were unable to develop targeted interventions for specific types of patients to more efficiently drive improvement. Furthermore, administrators could not see the correlation between risk and outcomes, nor could they track changes to the risk profile of the population over time.
In short, Mission had no way to see which interventions had an impact on outcomes for its bowel surgery patients so it could effectively drive improvement. It needed to design and successfully implement an organizational and analytics strategy to meet this need.
Mission devised a three-pronged strategy for achieving and sustaining evidence-based quality improvement for bowel surgery patients. This strategy involved:
Studies show that gaining widespread adoption of evidence-based protocols can be difficult, and organizations that successfully achieve higher levels of adoption have three things in common: they employ a collaborative approach, they standardize across the system, and they have access to and offer transparency of performance data.3 Mission’s success is attributable to incorporating those three elements into the bowel surgery initiative.
The creation of the bowel surgery CPM was a collaborative, interdisciplinary team effort, informed by the best available evidence and made as patient-centered as possible. By involving surgeons, nurses, pharmacists, therapists, social workers, and care managers in the development of the CPM, Mission was able to incorporate best practices for all disciplines and optimize everyone’s workflow. The use of engaged and active physician champions ensured that the team developed the CPM with the appropriated clinical oversight and that the resulting product was well understood and supported throughout the organization.
As Mission rolled the CPM out to additional hospitals across the system, it adjusted the plan to account for resource and volume differences while maintaining the standard processes.
The bowel surgery CPM consists of standard, evidence-based clinical protocols designed to provide guidelines that ensure that all bowel surgery care delivered throughout Mission—regardless of the patient’s location—is evidence-based best practice, patient centered, and delivered in the right care setting at the lowest cost to patients.
Key elements of the bowel surgery CPM include:
Evidence-Based Order Sets (Power Plans)
The bowel surgery Power Plan is a standard order set that generates consistent evidence-based orders while also allowing physicians to adapt care when necessary based on specific patient characteristics or needs. The Power Plan initiates all of the patient’s care and launches a standardized IPOC specifically designed for bowel surgery patients.
The interdisciplinary team developed Mission’s IPOC, which includes a nutrition plan, early mobilization, and other best practices for enhanced recovery after surgery. The team designed the IPOC in a way that supports multiple caregivers’ workflows and effectively standardizes and simplifies complex care for bowel surgery patients.
Previously, each surgeon had his or her own unique set of orders, making it extremely difficult for nurses or ancillary personnel to anticipate the care needs of patients. Having consistent orders and interventions makes interdisciplinary communication and workflow much more efficient and effective and improves the quality of care the patients receive.
The fact that ordering the bowel surgery Power Plan launches the appropriate IPOC for each patient has increased both physician and nurse satisfaction. Physicians know that when they order the Power Plan, their patients will get the support they need to heal and progress. The nurses know they will receive consistent and appropriate orders, including the protocols for enhanced recovery after surgery.
Patient Engagement and Healing Coaches
The bowel surgery CPM includes multiple strategies for engaging patients and families and educating them on practices that yield the best outcomes. Enhanced and targeted patient education begins at the physician’s office before surgery and continues post-discharge.
An important engagement strategy for the bowel surgery team is the use of Healing Coaches. The education materials given to patients during their pre-op visit at the physician’s office encourage them to find someone to act as their Healing Coach. The person they select—usually a family member or friend—will support them through their surgery and recovery.
Healing Coaches become members of the patient’s care team, helping with hand sanitization, post-operative breathing techniques, mobilization, and general patient support and encouragement. Mission gives educational materials to healing coaches to prepare them for their role in the patient’s care.
Mission has also employed post-discharge phone calls to help ensure patients understand their postoperative care plan. Nurses care managers call discharged patients to help identify any issues. Mission believes these callbacks will improve bowel surgery readmission rates.
The bowel surgery improvement team knew that no matter how good the CPM was, it would not change patient care or improve outcomes unless caregivers used the model consistently.
The team therefore decided to make it easy for providers to generate the bowel surgery Power Plan using the EHR and order entry system in conjunction with decision support. When physicians placed the order for the Power Plan, the system automatically generated the IPOC, thus making it much more likely that the best and appropriate care would be delivered to the patient.
Because the improvement team made it easier for physicians to do the right thing, and because physician champions spread the word about the CPM, Power Plan adoption rates rose quickly throughout the rollout.
Mission had already implemented an EDW platform to drive multiple performance improvement initiatives. The EDW aggregates clinical, financial, operational, and other data to create a consolidated view of data to inform decisions. Leveraging the power of the EDW would mean that the bowel surgery improvement team would not have to rely on the time-consuming, labor-intensive process of extracting data manually from the EHR and putting it into spreadsheets.
Having seen the advantages that a focused analytics application had on the work of other improvement teams, the team lobbied leadership to develop an application for the bowel surgery patient population. Mission therefore implemented an advanced analytics bowel surgery application on its EDW platform to inform the team’s improvement efforts and ensure ongoing compliance with the CPM (Figure 1).

Key benefits of the application are the ability to assess risk, measure outcomes, correlate interventions to outcomes, and watch for trends. Before these analytics were available, team members weren’t able to measure the impact of specific interventions on outcomes. Now, the application clearly shows that patients who receive the Power Plan have significantly better outcomes than those who do not.
Because Mission can show that patients whose care follows the Power Plan demonstrate significantly better outcomes than other patients, physicians are engaged to use the Power Plans. All of the surgery managers have access to this near real-time data and can get answers to important questions, drilling into the data without frustrating delays.
The CPMs are living, breathing, and always changing. The analytics application helps Mission understand what is happening with each component of the CPM, and enables the team to modify the plan based on the information. For example, when team members looked at readmissions data for bowel surgery patients, they found a spike on day two of discharge. They had originally targeted post-surgical unit RN’s to conduct follow-up phone calls to occur between 48 to 72 hours post-discharge, but, informed by the data, they changed the calls to occur within 24 hours of discharge. This change enables nursing staff to reinforce discharge education, identify potential complications, and provide direction to the patients regarding follow-up care needs. These strategies serve to reduce readmission rates.
By organizing a multidisciplinary improvement team, implementing an evidence-based care process model, and leveraging technology and analytics to encourage clinician adoption and deliver performance insights, Mission has achieved significant improvements in bowel surgery care.
One of Mission’s major goals for bowel surgery improvement was to reduce the infection rate among patients. Mission providers have been immensely successful in this effort, achieving an astounding 92 percent reduction in colorectal surgery SSI rates. The health system credits this reduction to use of the Power Plan and the associated IPOC, plus the institution of healing coaches.
As shown in the graphic below (Figure 2), Mission’s bowel surgery outcomes improved significantly when the Power Plan was used compared to when it was not, reinforcing the value of the care process model.
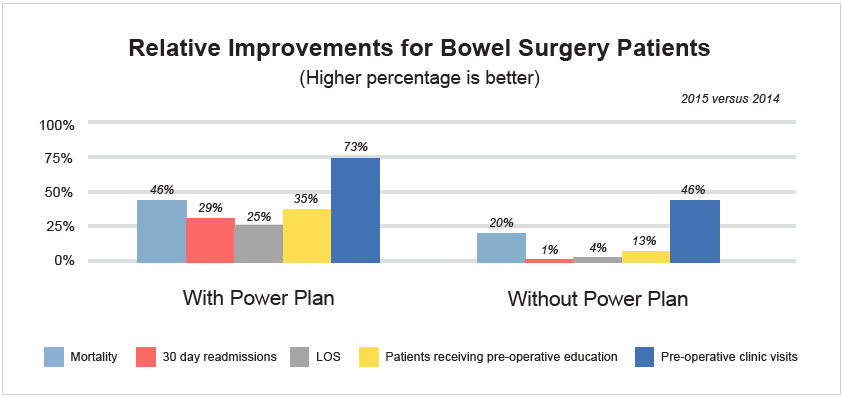
Between 2014 and 2015, a time when only 33 percent of Mission’s bowel surgery patients received the Power Plan, the improvement initiative yielded the following impressive results:
“Our care process model is an ever evolving model. It’s a living and breathing strategy that we are always looking to improve. That’s one reason why data is so important. It allows us to determine whether the CPM is really improving outcomes and to identify ways in which we could refine the model to make it even more effective.”
– Bonnie Nece, RN, Executive Director of Surgical, Services Clinical Programs, Mission Health
Determined to maintain the momentum of this initial success, the bowel surgery improvement team plans to continuously improve and broaden the use of the CPM and Power Plan. Ongoing patient and provider education will remain an important focus of the effort. Soon, Mission will implement a significant addition to its improvement program: a bowel surgery risk stratification model. This model will enable clinicians to proactively identify those patients at most risk for a complication or readmission and to focus the appropriate resources on their care, further improving clinical and financial outcomes.