Utilizing data and analytics, Hawai’i Pacific Health gained a deep understanding of its supply chain processes and data, allowing it to improve and maintain the reliability of this information, leading to meaningful and sustained improvements across the system.
Annually, U.S. hospital supply chain overspend costs an estimated $25.4 billion, which represents 30 percent of all hospital spending. Leaders at Hawai'i Pacific Health (HPH) understood the importance of improving supply chain data and its relationship to the organization’s financial health. However, siloed, inaccurate data from disparate sources inhibited the identification of meaningful improvement efforts. The health system worked to identify opportunities to reduce costs in the operating room (OR) supply chain across the organization, assembling a team to identify mechanisms for locating and reducing variation. Incorporating an analytics platform offered deeper insight into supply chain management and areas for improvement.
Approximately 30 percent of all hospital spending in the U.S. goes to supply chain overspend, which equals $25.4 billion each year. In hospitals, supply chain spending is second only to labor costs and is expected to rise.1
The supply chain interfaces with and impacts every department. Despite the interconnectedness of supply needs, goals and objectives are frequently misaligned across departments, resulting in siloed and inefficient supply chain management.2,3 The most discretionary type of spending involves medical and surgical supplies, and presents the greatest opportunity for process improvement. Top hospital performers consistently leverage evidence-based protocols and data analytics to reduce variation in pricing, product use, and clinical outcomes.1
HPH is one of the largest health care providers in Hawaii with four major medical centers and over 70 locations statewide. The provider’s mission is to create a healthier Hawaii through community outreach beyond the walls of its facilities as well as investments in research, education, training, and care for the underserved in the community.
While HPH leaders understood the financial importance of supply chain management, siloed and inaccurate data from disparate sources inhibited meaningful improvement efforts. Content expertise existed in the OR, supply chain, and master index, but the lack of consistent standard data definitions across the organization created a barrier between the OR and supply team groups, resulting in mistrust in the data and ineffective collaboration.
No standard process was in place for evaluating and purchasing new supplies. Over 100 new supplies were added monthly, making it difficult to match cost to supply. Many supplies were not identified and categorized as discrete values within the supply management system. Supply orders for the OR could be entered into the system by either selecting discrete values, or by free text data entry, creating barriers to tracking and aggregating information.
Preference cards, which are documented supply lists for each procedure that assist OR staff in setting up instruments and supplies as well as provide data to track costs and patient charges, were not standard and required a manual process to create preference cards for new providers. These cards were also inconsistent and often outdated. No dedicated person was responsible for updating and monitoring preference cards at either individual hospitals or systemwide.
The existing data left HPH unable to create logical or defensible supply chain solutions. To be successful at controlling supply chain costs long term, HPH needed to substantially improve the accuracy of its data. Inability to provide accurate data left clinicians in the dark and unable to help in efforts to reduce unnecessary spending.
HPH engaged with Health Catalyst to identify opportunities to reduce OR supply chain costs across the health system, assembling a team to identify mechanisms for locating and reducing variation. After extensive discovery work, it became clear that the data were not “clean” enough to drive improvement efforts, prompting the guidance committee to request the improvement team develop a plan to improve the foundational supply chain data and verify the validity of the data used for improvement.
Using the Health Catalyst® Data Operating System (DOS™) platform and a robust suite of analytics applications, HPH gained insight into supply chain management. The analytics platform integrates data from HPH’s EMR and multiple supply chain systems.
To manage and control supply chain costs over time, HPH recognized that it first needed to increase the amount of discrete supply documentation in the OR, improve preference card accuracy, and establish a request/review process for new supplies. With these efforts in mind, the organization established four separate workgroups to address four distinct opportunities within the OR:
These workgroups met weekly to identify tasks and next steps, collaborating to efficiently move work forward.
Throughout the improvement project, HPH engaged with and updated eight diverse stakeholder groups. Each one interacts with the supply chain data differently, and it is critical they be aware of any changes to source system data. To meet their varied needs, the team established formal communication plans, using standard messaging tools to convey changes to the source system data and associated processes.
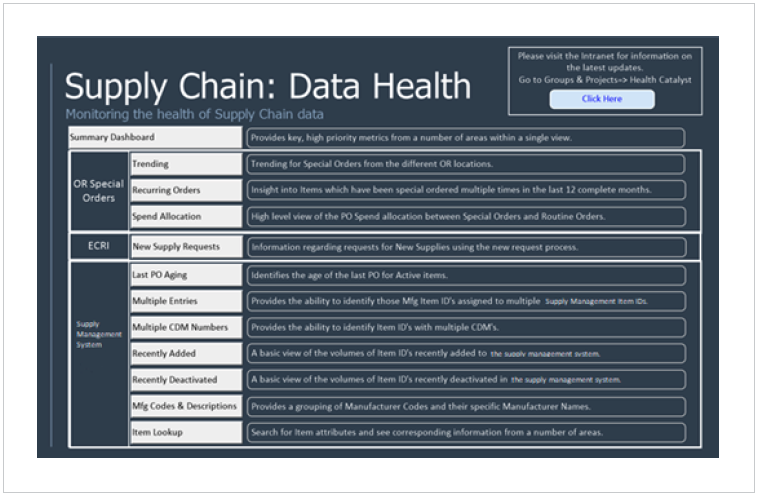
With standard data and processes in place, HPH and Health Catalyst collaborated to develop an analytics application. More than 100 users at HPH use this tool to aid their daily work as well as improve and maintain the “health,” or readability, of the supply data (see Figure 1).
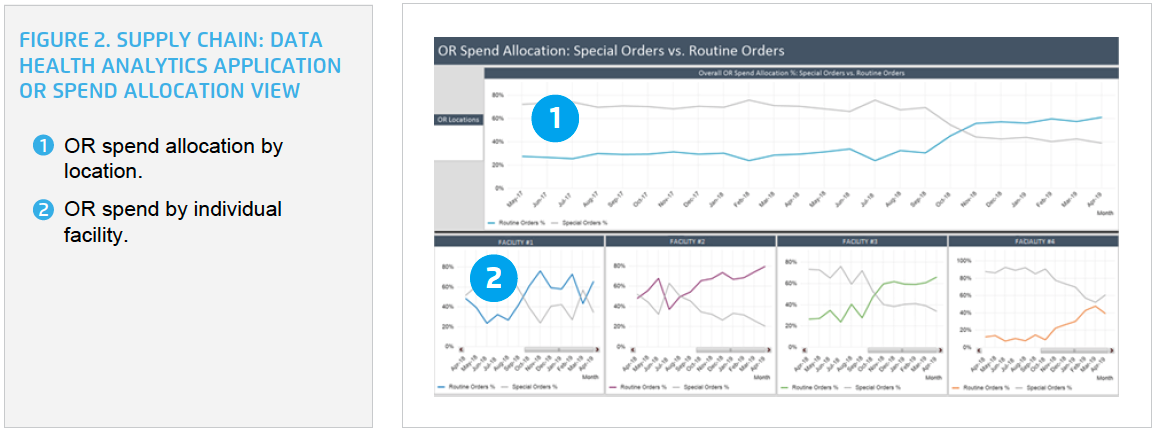
HPH can easily visualize the number of observed versus expected special orders, the difference in spend allocation for special versus routine orders, and quickly intervene to get the organization back on track (see Figure 2). HPH can drill into the data and easily obtain detailed special-order information for each of its four facilities.
HPH also uses the analytics application to monitor the new supply process, including the number of new supply submissions, the average days to a decision, and the amount of new supply requests by facility and review stream (see Figure 3).

HPH gained a deep understanding of its supply chain processes and data, which allowed it to improve and maintain the reliability of this information, leading to meaningful and sustained improvements across the system. In just six months, HPH has achieved the following results:
"This initiative has improved interdepartmental collaboration and trust. Additionally, HPH now has access to well-understood and trusted data that can be used to help drive improvement—reducing waste and controlling costs.“Access to meaningful, accurate data has helped improve credibility and increase physicians’ willingness to participate and reduce variation.”
– Liana Peiler, MD, MHCDS, Medical Director
HPH plans to ensure that processes and improvements are sustainable and replicable. Next, HPH will take on improving supply chain data in its other procedural areas, including endoscopy and the cath lab, and is preparing to implement activity-based costing.