An estimated 24 percent of patients who are discharged with heart failure (HF) are readmitted to the hospital within 30 days. Learn how this healthcare organization engaged physicians and multidisciplinary teams to improve outcomes. Deploying evidence best practices—medication reconciliation, follow-up appointments, follow-up phone calls, and teach-back—the organization reduced and sustained its 30-day and 90-day HF readmission rates.
Heart failure (HF) affects an estimated 5.3 million people, mostly the elderly, and is the underlying cause for 12 to 15 million office visits and 6.5 million hospital days each year.1 Because of inadequate treatment, discharge guidance, and follow-up, an estimated 24 percent of patients who are discharged are readmitted to the hospital within 30 days.2
Like most healthcare systems facing the transition to value-based reimbursement, this large healthcare system found it necessary to assess its overall quality improvement program. Leadership realized it needed to be able to analyze and better manage specific patient populations, especially patients with chronic conditions and those at greatest risk for readmission.
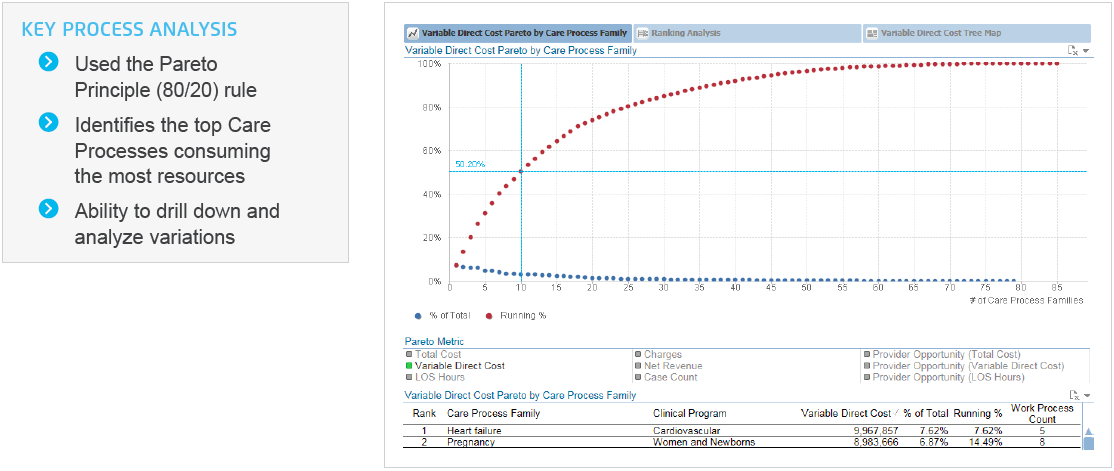
The Health Catalyst Key Process Analysis (KPA) Application identified heart failure as one of their highest cost care processes. The decision to begin its cardiac services improvement initiative by focusing on heart failure was a logical choice based on the KPA results and The Centers for Medicare & Medicaid Services (CMS) readmissions reduction program (Figure 1 sample visualization).
In 2014, CMS withheld up to 2 percent of regular reimbursements for hospitals that have too many 30-day readmissions for HF. The proposed rule for 2015 would increase the maximum penalty under the program to 3 percent. The healthcare system was determined to improve HF care for its patients and avoid CMS penalties.
The healthcare system initially deployed a traditional enterprise data warehouse (EDW) to help them in their quality improvement initiatives. But it found that this type of EDW took years to fully deploy and failed to enable the near-real-time analysis of clinical data required for success under value-based care. The healthcare system then turned to Health Catalyst’s Late-Binding Data Warehouse™, an agile platform that not only supports the fast- changing rules and use cases of healthcare data, but delivers value in a matter of weeks. The healthcare EDW was fully deployed within just 12 weeks.
The new healthcare EDW quickly pooled clinical, patient satisfaction, operational and other relevant data. To be successful, the Associate Chief Medical Officer and the Vice President of Business Intelligence knew they needed to engage physicians and build a culture of trust — through transparency and collaboration — and align on the vision of improved outcomes. They could choose to go fast, without clinician engagement. But they knew they could go further with the support of clinicians.
They organized a multidisciplinary team that included physicians, nurses, informaticists, quality, analytics, IT, operations and finance. The multidisciplinary team analyzed the pooled data using the Health Catalyst Key Process Analysis (KPA) Application. Armed with that insight and its new analytics capabilities, the healthcare system applied for and received a grant from a major foundation to support a transitional care program for heart failure patients. The center borrowed the grant’s objectives to defi its long-term AIM statement:
To achieve and sustain a 30 percent reduction in the 30- day and a 15 percent reduction in the 90-day all-cause readmission rates for patients with HF by [date] and sustained reduction in readmission rates through [date].
To achieve the goals set forth in its AIM statement, the multidisciplinary team worked together to define the patient cohort and to define four evidence-based, HF-specific best practice interventions, which were rolled out over a few months.
An integrated dashboard (Figure 2 sample visualization) was created in the healthcare EDW platform for each of the four interventions so clinicians and administrators could easily visualize the impact the changes were having on readmissions. Additionally, the healthcare EDW and the Population Health – Heart Failure Advanced Application allowed the multidisciplinary team to assess the interventions’ impact on costs and patient satisfaction.
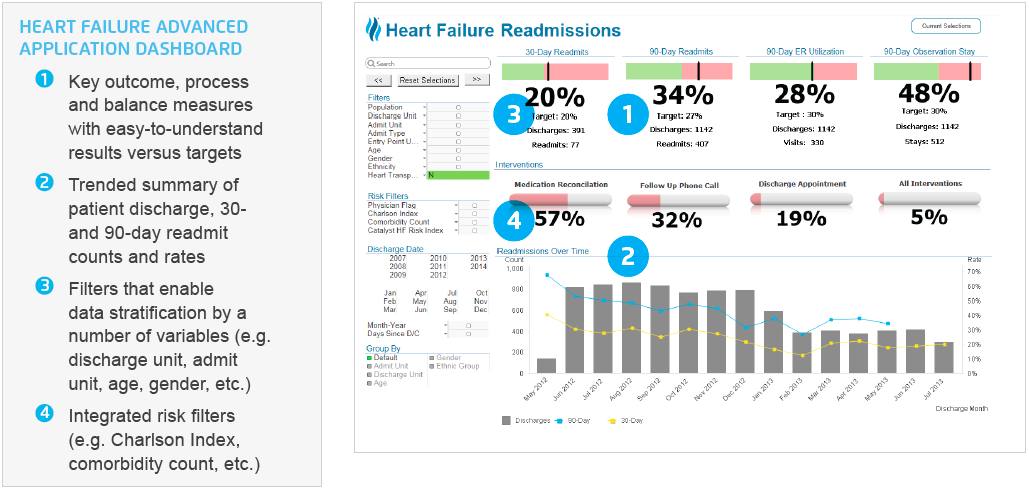
To ensure that the focus on reducing readmissions did not have an unintentional effect in other areas, such as an increase in emergency department (ED) visits or a decrease in patient satisfaction, the center built in balance measures including the tracking of ED encounters, observation stays, length of stay and patient satisfaction rates.
Eight months after implementing the four evidence-based interventions, the medical center had experienced a:

Population Health – Heart Failure Advanced Application also includes tabs for Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey results, length of stay (LOS) and cost analysis, and the ability to drill to the individual patient level.
“We have deployed evidence-based practices — medication reconciliation, follow-up phone calls and appointments, and teach back— to help reduce heart failure readmission rates. Analytics are enabling us to correlate our interventions with readmissions and trend readmissions over time for comparative purposes.”
– Associate Chief Medical Officer
As a result of these successes, the healthcare system is deploying the healthcare EDW, Health Catalyst Population Health Advanced Application, evidence-based practices — and its executive performance improvement governance structure and multidisciplinary team approach to manage the health of its employees and the patients it serves — and to drive and sustain performance improvement in a number of care processes including sepsis and infectious disease, and its general medicine, surgical and oncology clinical programs.