With the shift from fee-for-service to value-based payments, quality and efficiency are more critical than ever for hospitals. Discover how this hospital leveraged analytics, team-based processes, and evidence-based practices to transform its culture, optimize workflows, improve appendectomy outcomes, and reduce costs.
Approximately 250,000 cases of appendicitis occur every year in the United States. In fact, appendicitis is the most common acute surgical condition of the abdomen.1 These cases account for an estimated one million hospital days per year and consume 11.8 percent of all hospital discharges for gastrointestinal diseases.2
Research has shown that the mean length of stay (LOS) for appendectomy procedures can vary significantly based on a number of factors, including severity of appendicitis (e.g., simple, complex), operating room availability, surgeon preferences, nursing policies and hospital systems.3 Thus, ample opportunities to improve appendectomy care outcomes by streamlining processes and implementing evidence-based practices exist. Appendectomy care became an important focus for Texas Children’s Hospital, a not-for-profit organization consistently ranked among the top children’s hospitals in the nation, based on the large volume of appendicitis patients and the variation in practice. They also wanted to address the higher costs and increased morbidity related to severe (complex) appendicitis patients.
Texas Children’s has long recognized the importance of using technology to enable the delivery of higher-quality and lower-cost patient care. Quality and efficiency have become even more important to the hospital amid the impending transformation of the reimbursement system from fee-for- service to value-based payments. The hospital system is moving from cost-based reimbursement for Medicaid to a form of value-based payment under which hospitals that improve efficiency can keep the savings.
This case study details how Texas Children’s is using analytics technology, team-based processes and evidence-based best practices to drive higher- quality, lower-cost care for appendicitis.
Consistent with nationwide trends, Texas Children’s found that appendectomies represented one of their largest categories of surgical cases — with more than 1,000 appendectomy procedures each year. Based on the incomplete data they had gathered, they also discovered tremendous variability in LOS, costs and outcomes.
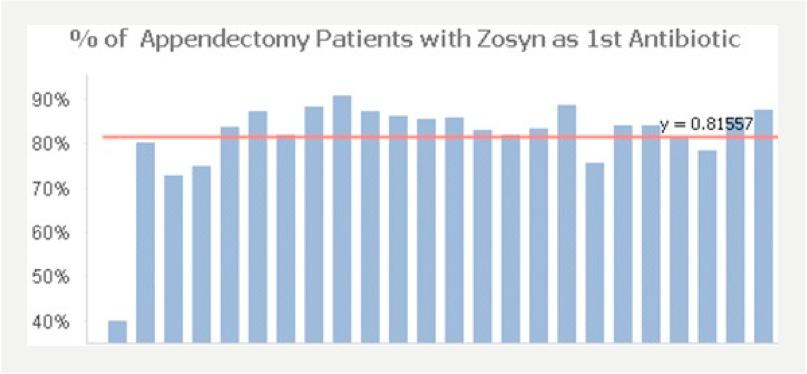
To improve costs and outcomes, the quality improvement team worked with the hospital’s Evidence Based Outcomes Center (EBOC), which develops evidence-based clinical guidelines to help clinicians manage the complexity of care and minimize variations in clinical practice. The team identified evidence-based practice guidelines and rolled them out among clinicians; however, there was no system in place to monitor outcomes after implementation of the guideline, or to track clinician adherence to the guidelines over time.
Another challenge Texas Children’s faced in improving appendectomy care was a lack of data. What data they had was delayed and retrospective and wasn’t gathered in a uniform, systematic way. The typical method for gathering the necessary data was for research residents and fellows to pull data from charts and analyze results. This effort was important in terms of generating answers to research hypotheses, but was not flexible or efficient in providing near-real time outcomes data necessary for guiding patient care. Additionally, it consumed resources and required retraining as residents completed their research rotations.
Texas Children’s turned to a technology-driven approach to enable its clinicians to deliver higher-quality and lower-cost appendectomy care. The hospital had already worked with Health Catalyst to implement a clinical, analytic and process-based framework for value-based transformation. This framework, known as the Three Systems Approach:
The hospital was using this framework to improve other clinical and operational processes, such as asthma care. They determined to apply these three systems to appendectomy care. Specifically, the program incorporated the following elements:
Because the permanent workgroup owns improvement for one particular care family over the long-term and is able to work with the EDW data in near real time via easy-to-use dashboards, they are successfully standardizing excellence in their care delivery work processes.
Although clinical transformation is an ongoing, iterative process, Texas Children’s appendectomy team has had impressive, measurable success in a short amount of time.
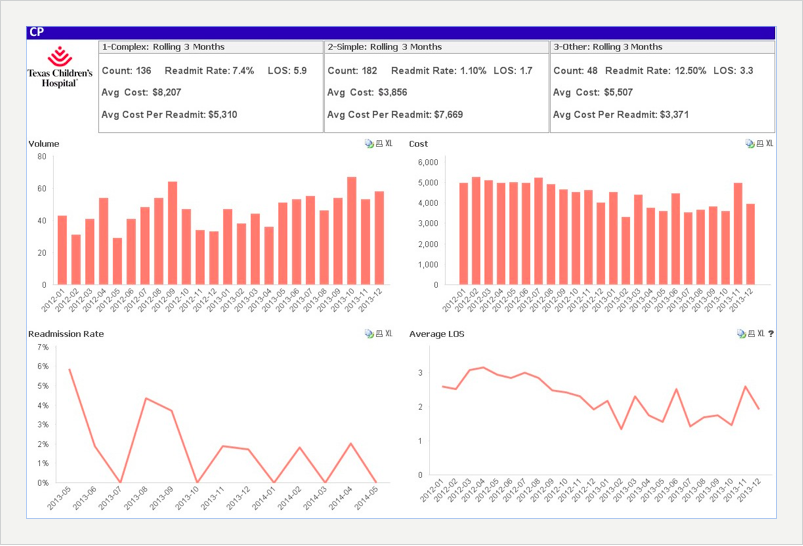
Using the EDW and the Appendectomy Module, Texas Children’s has developed a robust population health analytics platform for appendectomy care. Data from multiple source systems is now quickly integrated to enable prospective analytics in healthcare. This means that the team can assess outcomes for the population over an extended period of time and relate those outcomes to factors such as treatment protocols and suspected risk. Because clinicians were involved in developing the platform, they trust the data and use it as their single source of truth about appendectomy outcomes.
Visualizations available in the Appendectomy Module allow for easy identification of improvement opportunities and quick recognition of data quality issues. It is easy for individual clinicians and analysts to delve into the data themselves without having to request a report from the IT department. These clinicians and analysts are now able to compare data across all Texas Children’s locations where appendectomies are performed and stratify data based on patient characteristics such as age, gender, type of disease, etc. Prior to the EDW and Appendectomy Module, the team would spend several months just trying to collect the data.
In the Three Systems Approach that Health Catalyst advocates and Texas Children’s adopted, all systems — analytics, deployment and content — work together to establish an organization whose culture is one of data- driven improvement. The following results stem from the interaction of these three systems. Implementation of these systems results in a unique culture where clinicians on the frontlines of care use data and technology to make a difference in patients’ lives.
1. Cultural transformation
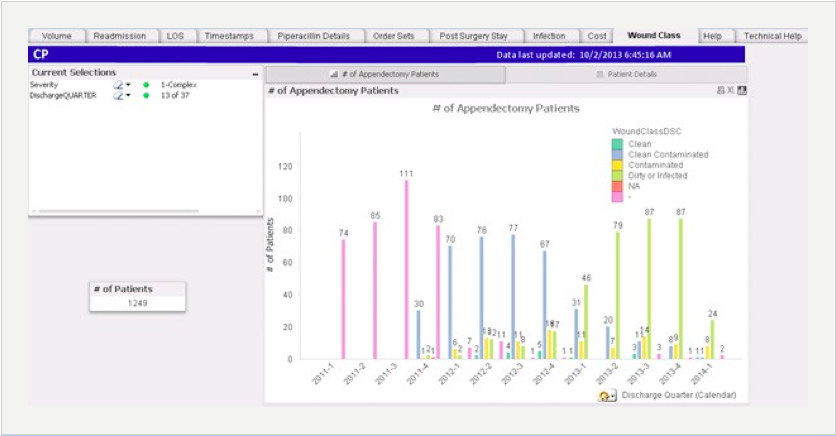
Combining a single, agreed-upon source of truth with clinician engagement enables the Texas Children’s team to use data in an ongoing cycle of continuous improvement. This effort has required concerted efforts to educate clinicians. Here is just one example of how engaging clinicians with data is driving cultural transformation. Surgeons are trained to document the severity of the case in the operative note. The team leverages an appendectomy visualization (sample shown in Figure 1) to estimate the number of severity changes that are made, which helps identify potential gaps in documentation.

As part of education and process improvement, the team trained the physicians on the operative note template. They share the metrics with physicians to establish an ongoing culture of transformation using data. Cultural transformation efforts have also involved nurse and family education.
2. Improved patient outcomes and reduced costs
Using evidence-based interventions and education, Texas Children’s has successfully improved outcomes from appendectomy surgeries while reducing costs. By creating standardized processes that follow evidence- based guidelines — and ensuring the adoption of these protocols across the enterprise — the hospital has realized the following positive year over year outcomes4:
The following are sample visualizations from the Appendectomy Module. The team uses these graphs and other visualizations to assess its quality and cost progress.
3. End-to-end workflow optimization
The team has mapped out workflow processes and is examining the amount of time required to perform each portion of the workflow: hours from presentation to diagnosis, diagnosis to surgery and surgery to discharge. Detailed data about workflow has enabled the team to understand differences in patient flow at their two campuses. Based on data, the surgical team worked with radiology to develop a standardized ultrasound reporting template that facilitated communication among providers ultimately reducing the time interval from diagnosis to surgery and leading to prompt disposition from the emergency department. They have also used seasonality data to help predict staffing during peak times. Through these efforts, they have decreased the time from presentation to diagnosis for simple appendicitis by two percent and decreased the time from diagnosis to surgery by 19 percent for the same types of cases.
"Establishing a single source of truth through the EDW has given us a shared understanding of appendicitis outcomes across the enterprise. Seeing what is possible with data is driving significant cultural transformation in our organization — and moving us into a new era of measurement.”
– Kathleen E. Carberry, RN, MPH, Director of Hospital Outcomes and Impact Service
The appendectomy team continues to identify opportunities to drive ongoing improvement and reduction in costs. And although Texas Children’s is using the Three Systems Approach to improve several clinical work processes throughout the enterprise, appendectomy is the first surgical procedure they have addressed. They plan to extend the methodology they have established to other surgical procedures.
As its storage of data about surgical performance grows, Texas Children’s plans to establish an unprecedented level of transparency with its community. The team hopes to post clinical outcomes — including complication rates — to its website so that families and patients can see what kind of outcomes to expect from the hospital. They also plan to train clinicians to use data to counsel patients and families as they face medical decision making dilemmas. One way Texas Children’s is doing this is through “outcome rounds” at the bedside with patients, nursing, surgeons and administration. Outcomes data are used during rounds to help answer questions from family members about their child’s clinical progress.




