Sepsis affects more than 750,000 hospitalized patients and results in 570,000 emergency department visits per year. Learn how this large medical center is tackling its sepsis care challenges by leveraging the EDW and healthcare analytics. The organization defined and built a sepsis registry and analytics platform in 10 weeks to measure six interventions and four outcome measures—including mortality rates, length of stay, total hospital stay and 30-day readmits.
Each year in the United States, approximately 200,000 people die from sepsis: systemic inflammation caused by severe infection. Sepsis affects more than 750,000 hospitalized patients and results in 570,000 emergency department visits per year.1
It affects not only patient health outcomes but also the overall cost of care. The average length of stay (LOS) for patients hospitalized for septicemia or sepsis is 75 percent longer than for those hospitalized for other conditions.2 In fact, of all inpatient conditions covered by every payer, septicemia has proved to be the most expensive. Treating patients with septicemia cost $20.3 billion in 2011, representing 5.2 percent of total inpatient costs.3
The public health magnitude of sepsis is clear. National and international public health organizations have developed programs to define sepsis and advocate improved care. The most notable of these is the Surviving Sepsis Campaign.4
Responding to the clinical and financial costs of sepsis, a large medical center is reengineering its processes and leveraging advanced healthcare analytics solutions to improve sepsis care. This health system is relying on data-driven care delivery to speed diagnosis and improve treatment for:
For three years, the health system had been working on improving its sepsis care processes, including developing a detailed care pathway for treating the condition’s different severity levels. One of the most difficult aspects of sepsis care is diagnosing it in a timely manner. The health system developed a program where the nursing staff completes a manual assessment of their patients on a regular basis, with the goal of identifying the onset of sepsis faster.
The assessment includes questions regarding potential infection and guides nurses through Symptomatic Inflammatory Response Symptom (SIRS) criteria. SIRS criteria include such things as:
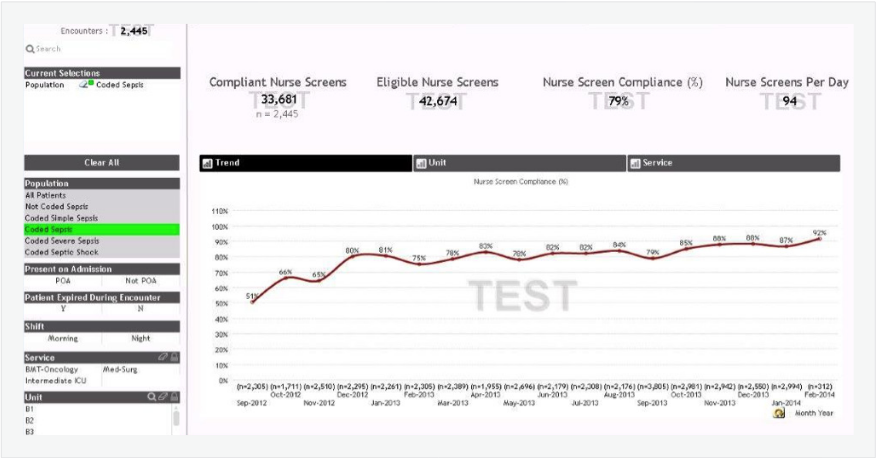
The manual assessment program was rolled out, but the health system lacked a system for measuring nurses’ compliance with the program. They needed a solution to track compliance with this important protocol.
After three years of work, the health system had been unable to develop an analytics platform that could establish baseline metrics and track the effectiveness of various interventions. To improve care quality and establish best practices, they needed a platform that could assess both the timeliness of care delivery and the impact on outcomes of interventions such as lactate tests and administration of antibiotics.
In the longer term, the health system sought to design a more efficient and accurate system for assessing sepsis. The sepsis nurse screening protocol relies on nurses cobbling together sepsis screening results every eight hours. They then have to notify a physician who may or may not proceed with the sepsis protocol based on his or her individual assessment.
Instead of relying on manual assessments, the health system wanted to develop an electronic algorithm for identifying septic patients. Such an algorithm would:
As an important component of its commitment to deploying best practices, the health system had already partnered with Health Catalyst to implement a clinical, analytic and process based framework for improving the quality and cost of care. The health system and Health Catalyst had established a healthcare enterprise data warehouse (EDW) that enables an enterprise-wide, consistent view of data from the EHR and other systems.
The health system chose to leverage this EDW as the analytics foundation for improving sepsis care. On top of the EDW platform, they deployed Health Catalyst’s Population Analytics Advanced Application- Sepsis Module. They also formed a cross-functional team of:
This team worked closely with the EDW and Sepsis Module to define cohorts, recommend best practices and assess electronic algorithm measurement variables.
The health system had been working on its sepsis project for three years with limited results. With Health Catalyst’s expertise and advanced analytics technology, they were able to create a sepsis registry and establish a sepsis analytics program in a mere 10 weeks.
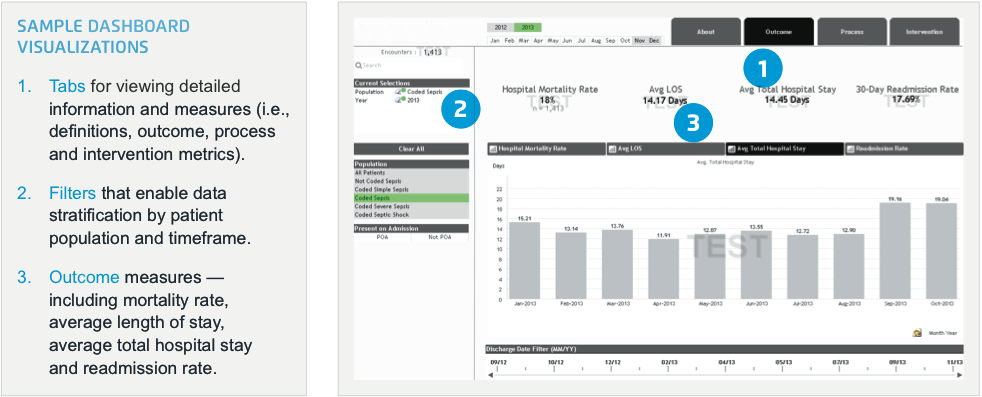
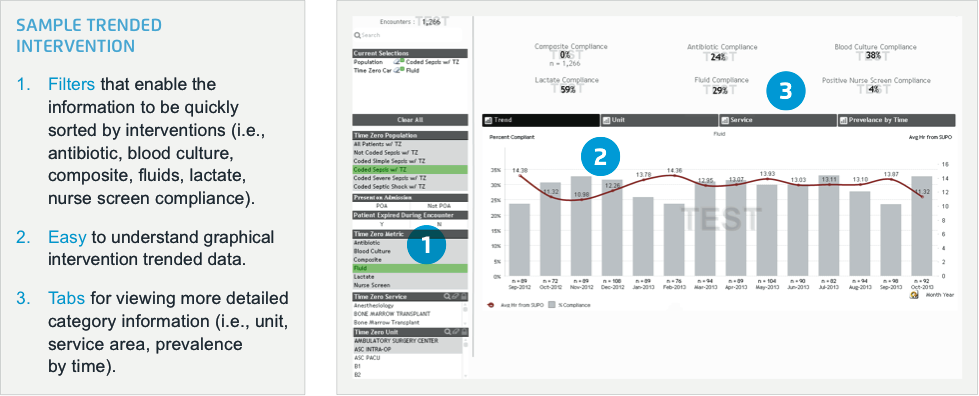
This scalable platform – that can integrate clinical, financial, operational and other data sources – will enable the team to track interventions and their impact on sepsis rates and financial measures. Organized around this analytics platform, the program now has consensus from the cross-functional team and a single source of truth on which to base assessments and future measurements.
The health system had implemented its manual assessment program with no method for assessing compliance. Now, with advanced healthcare analytics in place, they are able to track nurses’ compliance with completing assessments, as shown in Figure 1. Full compliance with the assessment program will increase timely identification of sepsis and aid in curbing its progression to severe sepsis and septic shock. The health system’s goal is to ensure that the screens are performed on each patient at the beginning and end of each nursing shift. They have realized an 80 percent relative increase in compliance – and a 41 percent absolute increase in nurses’ compliance with completing assessments.
Working closely with Health Catalyst experts, the health system has developed an electronic algorithm prototype for automating sepsis assessment. Leveraging the Surviving Sepsis Campaign’s International Guidelines for Management of Severe Sepsis and Septic Shock, the multidisciplinary team identified eight “suspected infections” (SI) and 32 “infection symptoms” (IS) believed to be indicators for patients with sepsis.
The challenge faced in developing the algorithm is to determine the most accurate combination of factors that will identify septic patients while mitigating false positives and false negatives. The team continues to evaluate the prototype. They will refine the algorithm until its accuracy is fully validated.
“We’ve been working with the idea of identifying sepsis baselines for almost three years. It’s hard to believe that now, in just 10 weeks, we have a platform in place to establish baselines, track compliance and measure how well our treatments are working. The electronic algorithm being developed will be an even bigger help to us.
It’s very difficult to diagnose the onset of sepsis in its early stages. This will allow us to identify sepsis more quickly and save patients’ lives.”
– Registered Nurse
With a baseline established and the analytics infrastructure in place, the health system is now ready to track the impact of interventions. Its first goal is to track the timeliness of the following interventions:
In addition to measuring compliance to intervention protocols, the health system will leverage the analytics system to evaluate the impact of interventions on mortality rates, LOS and direct costs.