Sepsis is a costly and often fatal hospital complication, with mortality rates between 20-50 percent. To combat this, hospitals use evidence-based care bundles. Mission Health improved its sepsis surveillance, increasing bundle compliance and decreasing unnecessary surveillance activities so staff can focus on other valuable patient care activities.
Sepsis acts swiftly and aggressively. Many sepsis patients ultimately progress to developing severe sepsis, and mortality rates are extremely high—between 20 and 50 percent.1 With severe sepsis striking more than 1 million Americans annually,2 the numbers are unacceptably high. The cost is also a burden on the U.S. healthcare system. Severe sepsis is the single most expensive condition to treat in the hospital, on average, costing over $20 billion every year.3 A major factor driving these expenditures is that the average length of hospital stay (LOS) for sepsis patients is 75 percent longer than stays for other conditions.4 In 2002, the international Surviving Sepsis Campaign was launched with the objective to decrease severe sepsis and septic shock mortality rates by 25 percent.5 Today, the campaign’s evidence-based 3- and 6-hour treatment bundles are widely implemented for improved sepsis patient care. The Centers for Medicare and Medicaid Services (CMS) has also stepped in. The National Quality Forum’s “Early Management Bundle for Severe Sepsis and Septic Shock” was scheduled to become a CMS sepsis measure that would take effect on January 1, 2015 for 2017 reporting. The measure has been revised and reissued, and hospitals are set to begin collecting data for this measure on October 1, 2015.
Hospitals like Mission Health are actively engaged in reducing sepsis mortality rates. The sixth-largest health system in North Carolina, Mission is on a continuous quest to implement quality improvements that enable every patient to achieve desired outcomes without harm, without waste, and with the best experience for the patient and family. Accordingly, Mission’s sepsis care team has implemented a number of best practices to safeguard patients from sepsis and quickly treat those who are diagnosed.
Mission had previously implemented effective evidence-based practices for Foley catheter removal, central venous catheters and peripherally inserted central catheter lines as well as measures to prevent hospital-acquired pneumonia and ventilator associated pneumonia, which often precede sepsis.6 An algorithm imbedded within Mission’s electronic health record (EHR) continuously monitors patients for early signs of sepsis, and automatically alerts caregivers when a patient screens at-risk. To treat patients with the condition, the team utilizes 3 and 6-hour bundle treatment regimens derived from the Surviving Sepsis Campaign.
With such concerted efforts in place, Mission’s sepsis mortality rates have consistently outperformed the national average. However, Mission wanted to reduce these rates and LOS even further. It also wanted to be prepared to readily meet future CMS reporting requirements. Both objectives called for a more systematic method of tracking and improving sepsis bundle compliance.
Optimal sepsis treatment is comprised of time-bound critical elements of care that, when strictly followed, can reverse this fast- acting condition. To track compliance with these bundle elements for optimal sepsis care in the past, Mission had used a manual process that was largely unsustainable and did not provide the level of detail necessary to identify key areas of opportunity and make further sustained improvements.
A care team coordinator spent roughly 15 hours a week reviewing charts, confirming sepsis diagnoses and tracking overall bundle compliance and individual compliance with each element of care—which included fluid resuscitation; lactate measurement; antibiotic administration within 3 hours; and two blood cultures drawn prior to antibiotic administration. Despite this time-intensive process, Mission’s care team had little insight into what might drive compliance challenges with individual bundle elements, as such detail was too cumbersome to manually uncover.
Because survival of sepsis is highly dependent on an early diagnosis, certainty that the EHR alert system was correctly flagging at-risk patients was another necessity. Yet it was difficult to decipher just how effectively the alert system carried out this critical task. As there are multiple ways to measure and code for the condition’s varying degrees of severity, Mission needed an effective way to combine ICD and DRG codes to accurately define and track the sepsis patient cohort.
Improving data quality would considerably mitigate all of the above issues and provide Mission’s sepsis care teams with the much- needed insight into performance improvement opportunities.
Mission already had the foundation in place to support access to such data: a late-binding enterprise data warehouse platform (EDW). As a platform that aggregates clinical, financial, operational and other data, the EDW is becoming the “single source of truth” for the organization, supplying the data for an array of analytics applications. To drive stronger sepsis surveillance and other quality improvements, Mission implemented an advanced sepsis analytics application.
From the general sepsis metrics tab (see Figure 1), care teams have an at-a-glance view of all major sepsis care metrics, including number of sepsis patients, mortality rate and sepsis LOS. Sepsis care team staff can also drill down and filter by severity, patient demographics, 3-hour bundle treatment elements, sepsis order set usage, and sepsis alerts. Comparative analysis is another new capability, such as comparing sepsis mortality by age group or a co-existing conditions.
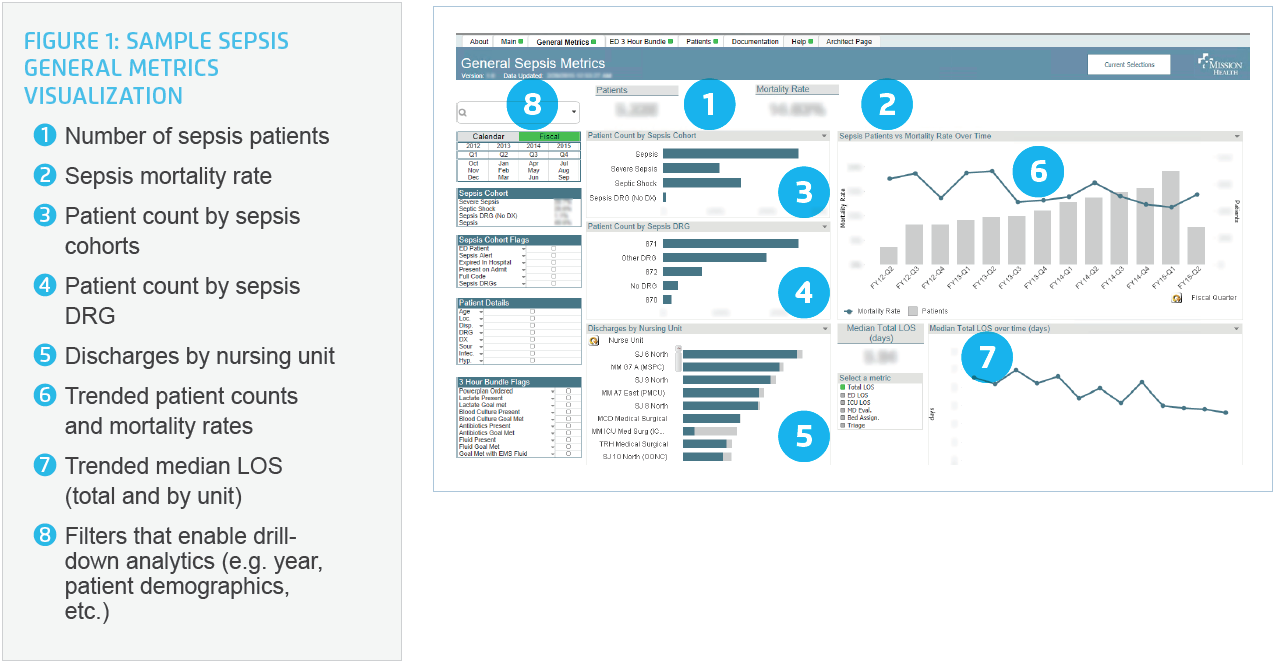
Trended visualization data allows for a quickly digestible assessment as to whether metrics are moving in the right direction. The visualization tool also gives new clarity on the sensitivity of the early alert system set up within Mission’s EHR. Care staff can now quickly see, for example, which severe sepsis patients actually received a sepsis warning alert to gauge how well the system is capturing patients; such insight reveals opportunities to improve early identification of at-risk patients.
With automation of the 3-hour bundle visualization (see Figure 2), the manual effort to track bundle compliance is no longer necessary. Instead, staff can focus time on analyzing root causes of compliance issues. As an example, staff can drill down to determine why antibiotic administration may be delayed. Perhaps it turns out that antibiotics were slow to be ordered, or the pharmacist was slow to verify treatment, or the nurse was delayed in administering it. The dashboard provides insight into several queries, including:
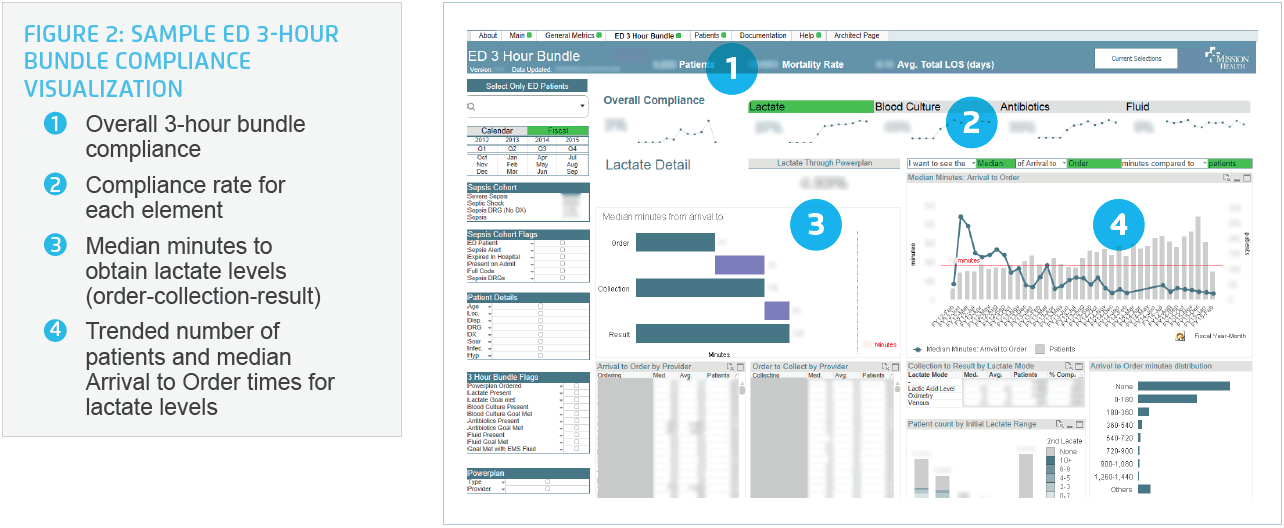
On the patient details tab, staff can pull a list of all sepsis patients currently in the hospital, and then drill down to individual cases to assess how well the best-practice bundle was met and how the patient subsequently responded to the treatment. Meanwhile, physician leaders can use the visualization as an educational tool by drilling into sepsis mortality and bundle compliance performance by individual physician. This supports transparent, data-driven conversations among physicians as to how sepsis care can be improved.
Through more widespread use of evidence-based interventions and education, Mission has successfully improved sepsis mortality rates and length of stay for severe sepsis patients.
The broadened education and access to data has resulted in meaningful care team engagement. One care team in the ED, for example, has committed to taking action at the bedside. With deepened understanding around the implications of delaying antibiotics, an ED nurse has taken ownership of regularly administering antibiotics to patients in under 10 minutes (an unprecedented speed).
12 percentage point improvement in overall bundle compliance rate in the ED. Compliance with all elements of care in the bundle have increased in the ED. For example, lactate compliance has increased 21 percentage points and antibiotic compliance has increased 12 percentage points
75 percent decrease in surveillance activities. The time- consuming manual chart reviews to confirm sepsis cases and examine bundle compliance have been greatly reduced. This is saving the sepsis clinical care coordinator about 15 hours per week, which can now be shifted to uncovering opportunities for quality improvements.
A significant contributor to this reduction in surveillance is the improved accuracy of the sepsis cohort definition. During the process of defining the cohort by using data from the EDW, the team realized that a significant portion of sepsis patients had been unintentionally excluded from the cohort. While these patients had a DRG code for sepsis, an ICD code for sepsis did not exist in their chart.
By leveraging the late-binding nature of the EDW, sepsis could be defined as broadly as possible to capture all sepsis patients. Mission was now able to define sepsis in multiple ways through a combination of ICD and DRG codes to create an accurate, comprehensive picture of its sepsis patient population.
“Five years ago, the only way we’d see improvement opportunities for sepsis care was at formal meetings or if cases were proactively brought to my attention. With the sepsis analytics, now we have all this insightful information. At any time we can drill down to the most meaningful metrics at the patient and provider level. I expect significant improvements in sepsis care to be made with this new access to data.”
– Scott Ramming, MD ED Physician
Mission is in the midst of an even broader rollout of the sepsis application. As physicians begin to use the tool to track and access their performance and compliance to the bundle, sepsis patient outcomes are expected to improve even further.
In addition to tracking and improving compliance with the 3-hour sepsis bundle, Mission is now well positioned to do the same with the 6-hour sepsis bundle. Indeed, Mission is prepared for the sepsis protocol and CMS reporting requirements that will begin on October 1, 2015—with minimal manual work.