For healthcare organizations, the ability to analyze problems and implement timely, effective improvements is necessary to maintain a competitive advantage, requiring a consistent, systematic approach to introduce and implement change. By developing a new strategy focused on uniform adoption, education, and ongoing oversight, Community Health Network changed the way it approached all organizational improvement efforts.
For healthcare organizations, the ability to analyze problems and implement timely, effective improvements is necessary to maintain a competitive advantage. An important component of successful, permanent improvement is using a consistent, systematic approach to introduce and implement change within an organization.
Community Health Network (CHNw) had invested in training caregivers on several improvement science models. However, improvement efforts at CHNw were often siloed and not widely spread across the organization, contributing to a lack of sustainability. By developing a new strategy focused on uniform adoption, education, and ongoing oversight, the organization aimed to change the way it approached all organizational improvement efforts going forward. CHNw has experienced impressive early adoption of its systematic improvement approach, and the new structures are already bringing value to the organization.
The ability of healthcare organizations to change, adapt, and evolve is a competitive advantage.1 More than half of health IT leaders report that it is difficult to consider new technologies that require substantial changes across disciplines, even when the technology has the potential to improve patient care and satisfaction.2 Successful and sustained improvement requires a consistent approach to the introduction and implementation of change within an organization.3 Single improvement approaches are not meant to replace change methodologies or tools used by organizations, but rather to provide a framework for analytics, organizational collaboration, and feedback to remove barriers and accelerate outcomes.4
CHNw is a non-profit healthcare organization, serving central Indiana. It is consistently ranked among the nation’s most integrated healthcare systems. Based in Indianapolis, CHNw serves more than 539,000 patients and employs over 15,000 caregivers, providing access to exceptional healthcare services, where and when patients need them—in hospitals, health pavilions, and doctor’s offices, as well as workplaces, schools, and homes. CHNw values patients first and is committed to providing patient-centered care and outstanding service, delivered with respect and compassion.
Previously, CHNw had invested in training caregivers on several improvement science models, such as lean production, Six Sigma, and change acceleration strategies. However, improvement efforts were often siloed and not widely spread across the organization. Without a common improvement approach, the organization had many well-intended projects, but a lack of governance and inefficient resource utilization reduced the potential effectiveness of improvement efforts.
Because CHNw lacked actionable data, it was difficult for the organization to identify and prioritize improvement efforts. To facilitate sustainable improvements, CHNw needed to change and better organize its improvement efforts to ensure widespread adoption across the organization.
CHNw leadership established a vision for quality, aiming to deliver an exceptional experience to every life it touches. The organization describes quality as defined by its individual patients, based upon outcomes, experience, cost, and the appropriateness of care. CHNw partnered with Health Catalyst, implementing improvement functions in three systems to achieve systematic, organization-wide change.
With this support, CHNw was able to adopt a consistent, systematic improvement methodology across the organization. This consistency in problem-solving and improvement provides a common language and sequence of steps for reaching goals, effectively establishing best practices across CHNw.
The improvement approach CHNw selected is compatible with multiple improvement methodologies, including Six Sigma, PDCA, DMAIC, and design thinking. It was important that the strategy be agile and adaptive, allowing teams to navigate improvements in an iterative fashion by moving quickly through some phases, or revisiting earlier steps as needed to ensure a positive outcome.
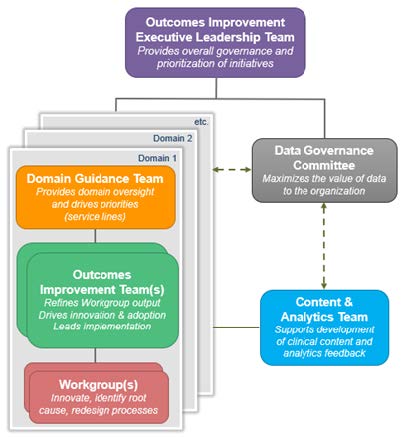
With the improvement approach in hand, leadership established a governance structure and commissioned permanent improvement teams to help achieve key organizational priorities and goals. CHNw’s governance structure integrates several important principles, including:
The permanent improvement teams are fully resourced, and the initiatives they spearhead are prioritized above other improvement efforts due to their alignment to strategic objectives. The permanent improvement teams also support ongoing efforts with representation from the necessary organizational functions, including outcome performance managers, financial analysts, clinician champions, and executive sponsors, to ensure organizational changes are widely adopted (see Figure 1).
Data analysts and CHNw outcomes and performance managers facilitate data-driven improvement, leveraging data from Health Catalyst Data Operating System (DOS™) platform to generate new insights. Clinical leadership views data and analytics as strategic asset, helping to drive adoption and accelerate improvements. When facing challenging organizational problems, CHNw asks and answers seven critical questions:
Coordinated training was provided for leaders across the system through in-person meetings and written materials. Leaders are encouraged to use the framework for improvement innovations within their service lines. Once prioritized and selected, projects are deployed to the permanent improvement teams to begin the improvement process.
This consistent, systematic, and widespread improvement approach provides CHNw leaders with a comprehensive repository of projects across the network, enabling status reports and ongoing resource allocation so that all future initiatives have a great chance for success.
The consistent, systematic improvement approach has begun to accelerate improvement at CHNw. The health system has experienced impressive early adoption of its improvement approach, and the new structures are already bringing value to the organization. In just two years, CHNw has:
The improvement teams are delivering impressive results. For example:
“Rather than rushing to a solution, leaders are now applying the improvement framework to both small and large problems, pausing to be certain we know the problem we need to solve, and focusing their improvement efforts on the processes associated with the problem.”
- Patrick McGill, MD, EVP, Chief Analytics Officer
Having established a consistent improvement approach supported with data and analytics, CHNw intends to further expand its data literacy and expand its use of analytics to drive improvement, and plans to further reduce clinical variation, improving the quality of care delivered to patients.


$15.5 million in savings, including: