Community Health Network (CHNw) was keenly aware of the needs of the elderly population in its communities of impact. However, despite the development and implementation of a successful geriatric program, the organization lacked access to, and visibility of, meaningful data to quantify program outcomes. The CHNw Geriatric Evaluation and Management (GEM) team used an analytics application to demonstrate the sizeable, positive impact of the GEM team care and interventions on both patient and financial outcomes.
Today, individuals over the age of 65 make up 13 percent of the U.S. population but account for 43 percent of inpatient hospital stays. The 65-and-over population is projected to nearly double over the next three decades, from 48 million to 88 million. As the U.S. population ages, health systems must accommodate the expanding healthcare delivery demands of aging communities.
Community Health Network (CHNw) was keenly aware of the needs of the elderly population in its communities of impact. However, despite the development and implementation of a successful geriatric program, the organization lacked access to, and visibility of, meaningful data to quantify program outcomes. Without data, funding for the geriatric program remained at risk.
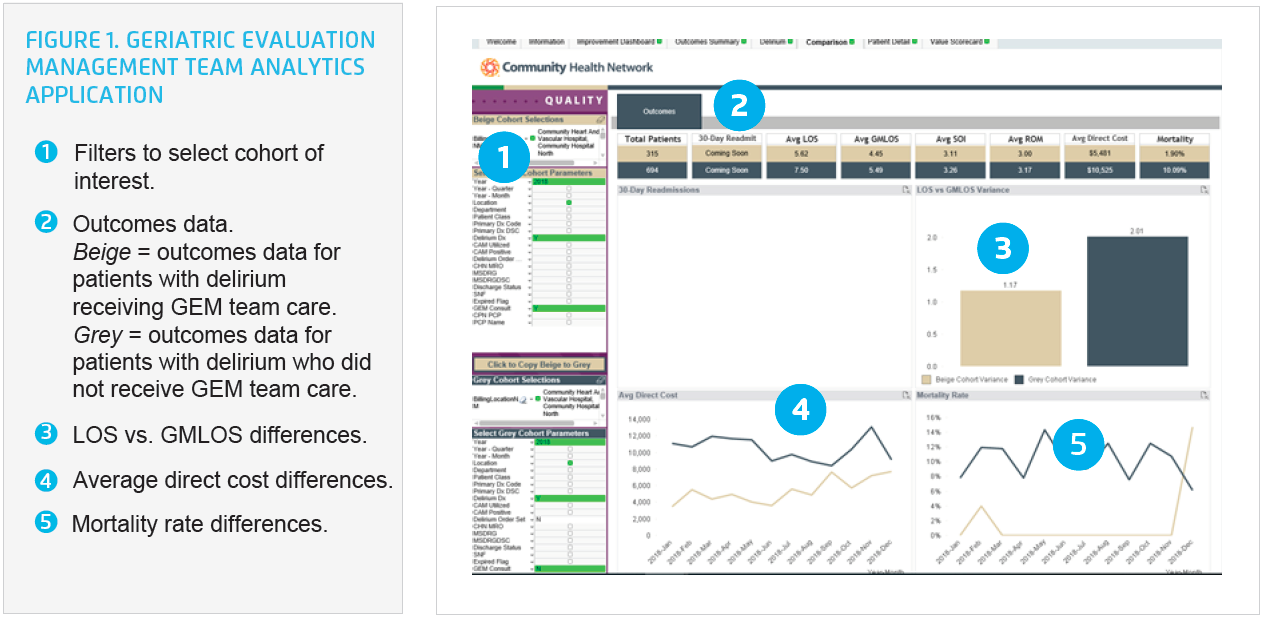
To generate the needed data, the CHNw Geriatric Evaluation and Management (GEM) team used an analytics application to demonstrate the sizeable, positive impact of the GEM team care and interventions on both patient and financial outcomes.
In the U.S., individuals over the age of 65 represent only 13 percent of the population, yet they account for 43 percent of inpatient hospital stays.1 The 65-and-over population is projected to nearly double over the next three decades, from 48 million to 88 million, placing growing demands on the nation’s healthcare system.2
The industry tenets of inpatient geriatric care are based on the Acute Care for Elders (ACE)3 model that recognized mobility and orientation as crucial components of elder care, and the Nurses Improving Care for Healthsystem Elders (NICHE)4 initiative, an evidence-based best-practice resource. The core of inpatient geriatric care relies on avoiding a decline in physical frailty and cognitive impairment, which are both linked to an increase in functional decline, morbidity and mortality, and higher healthcare costs.
A non-profit healthcare organization, serving central Indiana, CHNw is consistently ranked among the nation’s most integrated healthcare systems. Based in Indianapolis, CHNw serves more than 539,000 patients and employs over 15,000 caregivers. It delivers exceptional healthcare services, where and when patients need them—in hospitals, health pavilions, and doctor’s offices, as well as workplaces, schools, and homes. CHNw values patients first and is committed to providing patient-centered care and outstanding service, delivered with respect and compassion.
In response to the projected exponential growth of geriatric healthcare needs, the CHNw executive team identified improving geriatric care as a potential service differentiator in the market. The team recognized that, in general, geriatric models are resource heavy due to the complex needs of that population cohort.
Based on the recommendations from the Enhanced Care for the Elderly Working Group, CHNw established a multidisciplinary GEM team, as a mobile hybrid of the ACE inpatient model, and linked to NICHE best-practice evidence, standards, and training principles. Optimal care required an interdisciplinary team, including physicians, advanced practice providers, registered nurses, social workers, and pharmacists, in addition to multiple modes of therapy.
CHNw had difficulty quantifying the time, resource, and staffing requirements to manage the needs of geriatric patients and their families and linking those factors directly to program outcomes. To secure continued funding for the GEM team, the organization needed to balance the cost of resources with the cost of the program and demonstrate financial viability. Unfortunately, when the GEM team first started as a pilot, they lacked the data to demonstrate the program’s effectiveness and positive impact on patient outcomes because they were a new program to the network.
The health system needed a single source of truth with which to compare program participant outcomes to non-participant outcomes. Data from the EMR proved insufficient for tracking patients receiving care from the GEM team and their outcomes, as the organization struggled to get meaningful performance data out of the EMR and tie that data to financial performance.
To evaluate outcomes, GEM team leaders manually tracked the patients who had received GEM team services in a spreadsheet. They spent at least 30 minutes updating the spreadsheet each day. They would then hand the spreadsheet off to a colleague in finance, who would spend several hours each month attempting to use the data to determine the cost of the program and identify any financial improvements. Limited aggregate data was available, but the data was three- to four-months-old. The age of the data and the manual entry led many to question the data’s validity, decreasing its value for ongoing improvement and program evaluation.
CHNw recognized the benefits of the GEM program, but without measurable outcomes that could be shared to demonstrate the improved health outcomes and reduced costs associated with the program, future funding for the program remained somewhat at risk.
Aware of the importance of evaluating program outcomes, GEM program leaders reached out to the executive team, requesting CHNw include the GEM program in its systemwide improvement methodology—establishing the team as a formal improvement team and prioritizing the allocation of resources to develop meaningful analytics to enable the team to perform comprehensive program evaluation. The executive team saw the value of allocating resources for this purpose.
To meet the robust analytics needs of the GEM program, CHNw leveraged the Health Catalyst® Data Operating System (DOS™) platform and a robust suite of analytics applications. This established a single source of truth for the GEM program and supported a GEM analytics application to meet the unique data needs of the GEM team.
Clinicians, analysts, and finance experts worked together to select the key performance indicators (KPIs) to include in the application and collaborated to validate the data for the analytics application. CHNw is now able to visualize data and outcomes for patients receiving care from the GEM team, including KPIs such as length of stay (LOS), readmission rates, financial data and costs, mortality rate, and medication use.
Through the analytics application, providers, advanced practice providers, registered nurses, case managers, therapists, pharmacists, data analysts, financial analysts, and leaders have access to near real-time, actionable data to guide decision making and help improve patient outcomes. Rather than waiting weeks or months for data, the team can now easily review up-to-date performance data each day.
Delirium, for example, is a major contributor to increased LOS, poor patient outcomes, and increased mortality rates. The analytics application supports program leaders in comparing, monitoring, and improving outcomes for patients with delirium who are receiving care from the GEM team, and supports the leaders in comparing those outcomes to patients with delirium who did not receive care from the GEM team. (see Figure 1).
The health system can evaluate the program’s impact on the total cost of care and cost avoidance, which is increasingly important in an era of value-based care and critical for programs like GEM, which are resource heavy with costs that may not match the revenue received for the acute care stay. The ability to measure the impact of these programs on cost avoidance and downstream revenue is often the key piece of data that helps ensure continued program funding.
Using the analytics application, CHNw can easily identify acute and post-acute resource utilization. The organization can evaluate the number of patients who receive rehabilitation services, speech therapy, and consults from the dietician. It can evaluate the number of new diagnoses added after GEM team engagement, such as improved recognition of malnutrition, as well as monitor and evaluate the number of patients discharged to skilled nursing care, to hospice, or to home; the number of palliative care consults; and the number of referrals across the care continuum.
In cultivating a data-driven, transparent environment, CHNw has given appropriate access to the analytics application and associated data to the team members involved in geriatric care—access is not restricted to only those members of the GEM team. All team members involved in the care of geriatrics patients can easily obtain the information needed for continuous improvement. Up-to-date, timely data and analytics increase transparency, and the rapid visualization of clinical, financial, and operational outcomes enables a comprehensive evaluation of the costs and benefits of the GEM program.
Using the analytics application, the GEM team demonstrated the sizeable, positive impact of its team care, and interventions on both patient and financial outcomes. The GEM team achieved the following meaningful results:
The analytics application has also improved operational efficiency. Previously, teams were spending hundreds of hours a year manually updating spreadsheets in an attempt to track and evaluate patient outcomes. With automation, teams can direct those hours back to patient care, further improving the effectiveness of the GEM team and improving the care the team provides to the patients it serves.
Analytics has demonstrated the effectiveness of the GEM team and the positive impact the GEM team has on patient outcomes, financial outcomes, and operational performance. The improved visibility into performance has built the health system’s confidence that it is investing its resources into the right program, ensuring ongoing program viability.
“For program success, there needs to be a partnership between clinicians and finance. Our improvement framework helps to align both groups, and the analytics application includes the finance and clinician approved data and outcomes.”
– Mark Pfeifer Senior Financial Analyst
CHNw plans to further improve the care it provides to geriatric patients and is working to improve the identification of patients at risk for delirium and increased frailty. The GEM team recently completed a pilot program for improving delirium screening outside the ICU, increasing the number of patients with delirium who receive the appropriate nursing care plan and provider order set. The organization has also adopted the American Geriatric Society Beers Criteria® as a guideline for medication prescribing for the geriatric population. The next phase of the GEM program will be to work on expanding delirium prevention and screening outside of the ICU, as well as reduce potentially inappropriate medication use in the GEM population.




