Texas Children’s Hospital is improving the care delivery of its patients with diabetes, one of the most common diseases in school-aged children. How? Powered by dedicated improvement teams and analytics, they have focused on order utilization, timeliness of IV and subcutaneous insulin administration, length of stay (LOS), establishing a diabetic care unit (DCU), educating core diabetic nurses (CDNs), frontline staff adoption, and more.
Diabetes mellitus is one of the most common diseases in school-aged children. In fact, in 2012, more than 200,000 young people in the United States under age 20 suffered from the disease.1 Unfortunately, the number of children and adolescents in the U.S. with type 1 or type 2 diabetes is increasing.2
This growing incidence of diabetes has significant ramifications for children’s long-term health, since the disease at least doubles a person’s risk of early death.3 It also poses a real quality and cost challenge for hospitals. Diabetes can be difficult to manage in the hospital because acute illness, surgery, and changes in daily routines can affect blood glucose levels.4 Furthermore, diabetes patients are at risk for serious complications, longer hospital stays, and poorer outcomes.5
A particularly complex and serious complication of diabetes is diabetic ketoacidosis (DKA). A condition that can result in diabetic coma or even death, DKA is a leading cause of morbidity and mortality in individuals with type 1 diabetes.6 Managing complex patients with DKA requires a dedicated effort on the part of health systems to ensure that caregivers have the best possible skills, knowledge, and resources.
One health system committed to improving care for patients with diabetes, and particularly DKA, is Texas Children’s Hospital. Internationally renowned for excellence in pediatric care, Texas Children’s provides primary and tertiary care for children through hospitals, affiliated practices, and a health plan.
Texas Children’s clinical and operational leaders noted a measurable degree of variation in its management of patients with DKA. This variation had been increasing over several years, leading to gaps in quality of care for patients admitted with DKA. Texas Children’s determined to reverse this trend by launching an enterprise-wide campaign to drive diabetes care improvement.
As Texas Children’s leaders assessed quality and cost outcomes, it became clear that diabetes care met the major criteria for a focused improvement effort: A large enough population of patients, a high degree of variation in care, measurable gaps in the consistency and quality of care, and organizational readiness. This last criterion was perhaps the most important. Not only were staff and faculty trained in quality improvement, they were also hungry for change that would lead to better diabetes care. The health system had the physician experts required to treat patients with DKA effectively; it simply needed to standardize and expand the scope of care to provide the comprehensive treatment that patients with DKA needed.
Texas Children’s kicked off its improvement initiative with an effort to standardize care through a set of evidence-based care guidelines for the management of DKA. Interdisciplinary teams developed these standard, evidence-based order sets designed to promote greater consistency in care from patient to patient. Unfortunately, with no implementation team to ensure their adoption, leaders quickly discovered that clinicians were not using these order sets consistently. Adoption of the new order sets was too dependent on “passive uptake”; therefore, too many disparate order sets remained in use.
Texas Children’s also found that a lack of data hampered its efforts to measure progress and implement continuous improvement. Data was available, but data extraction was too dependent on time-consuming manual processes that were not nimble enough to support rapid cycle process improvement, and the data was not making it back to the providers or frontline staff who were capable of making changes to care delivery. The health system also lacked established, agreed-upon metrics for DKA care, which were needed to guide the improvement effort. In short, despite interest and collaboration among caregivers, Texas Children’s did not have a systematic way to implement and sustain improvements in the care of diabetic patients.
Texas Children’s leaders established the Inpatient Diabetes Care Process Team (CPT), a physician lead, interdisciplinary team, comprised of endocrinologists, pathologists, emergency and intensive care physicians, registered nurses from the inpatient arena, emergency center, and ICU, and pharmacists. The Inpatient CPT is dedicated to improving the care for patients with diabetes who are admitted to Texas Children’s hospital, and committed to leading Texas Children’s inpatient diabetes improvement initiatives. To establish a foundation for systematic, sustainable improvements in diabetes care, Texas Children’s implemented the Health Catalyst Analytics Platform built using the Late-Binding™ Data Warehouse architecture (EDW). The EDW integrates data from internal sources like the EHR, financial systems, operational systems, and more.
Texas Children’s also implemented a pediatrics diabetes analytics application, which pulls near real-time data from the EDW. The application makes accurate, timely data available to the Texas Children’s team to support continuous diabetes care improvement. It allows the diabetes team to analyze performance, discover the root cause of problems, and identify opportunities for improvement.
Team members recognized that incremental change would not suffice to achieve this far-reaching goal. Instead, they would have to transform completely diabetes care throughout Texas Children’s facilities. Such transformation would require changes in two veins:
The team developed a diabetic care unit (DCU) for the care of its patients with DKA. The DCU ensures that patients with DKA receive comprehensive, evidence-based care and education based on their acuity and support needs. Providers that specialize in diabetes care staff the DCU. Patients who would have otherwise been admitted to the pediatric intensive care unit (PICU) to receive care are able to receive safe, highly specialized care in the DCU. The DCU also reduces variability in care by establishing standard work in areas such as patient education and care team/family meetings. Particularly important among the staff of this new specialty unit are Core Diabetic Nurses (CDNs) with extensive and ongoing initial training in diabetes management. The CDNs lead efforts on the DCU to deliver care and education 24/7 to meet the needs of patients and families.
Reengineering the care process required Texas Children’s to standardize care on evidence-based guidelines. As a means to guide effective implementation of these changes and to manage, monitor, and measure progress toward its goal, the team created a series of goal statements. The principal goal statements focused on the following:
Rapid recognition of DKA in the emergency center: To facilitate rapid identification and treatment of DKA in the emergency center (EC), the Inpatient CPT collaborated with physicians, registered nurses, and leadership in the EC to improve the number of patients who receive capillary point of care ketone testing in triage. The presence of ketones differentiates between a hyperglycemic event and life threatening DKA. Rapid identification of DKA in triage results in more timely treatment, decreasing the time a patient needs to spend in the EC, and decreasing the total LOS. To ensure that timely treatment is provided to patients experiencing severe DKA, the Inpatient CPT worked closely with pathology, using the data in the EDW to review historical ketone values and pH levels for patients who were previously treated for DKA. Working together, they established a correlation between point of care ketone values and pH levels, and established a specific ketone value that is indicative of severe DKA and results in immediate medical management of the patient in the EC.
Order set utilization: The team solicited stakeholder involvement, and successfully reduced its 10-15 existing order sets down to a standard group of four evidence-based order sets (DKA ER, DKA non-ER, non-DKA ER, and non-DKA non-ER) that are continuously evaluated and refined. The streamlined order sets simplify the care process for the clinicians, and reduce order entry errors, making it easier to navigate the complexity of inpatient care for diabetes.
Importantly, because of the way the order sets are built into the EHR, it is hard—and, indeed, almost impossible—for care providers not to use them. For example, it is now difficult to order insulin without using the standard order sets.
Timeliness of IV insulin administration: Clinical evidence indicates that timely administration of IV insulin significantly raises the quality of care for patients with DKA. Therefore, the Texas Children’s team developed and built into the EHR a standard, evidence-based protocol for the dose, method, and approach to ordering and administering IV insulin. The EDW and analytics application enables the team to measure compliance with this protocol and subsequent quality gains.
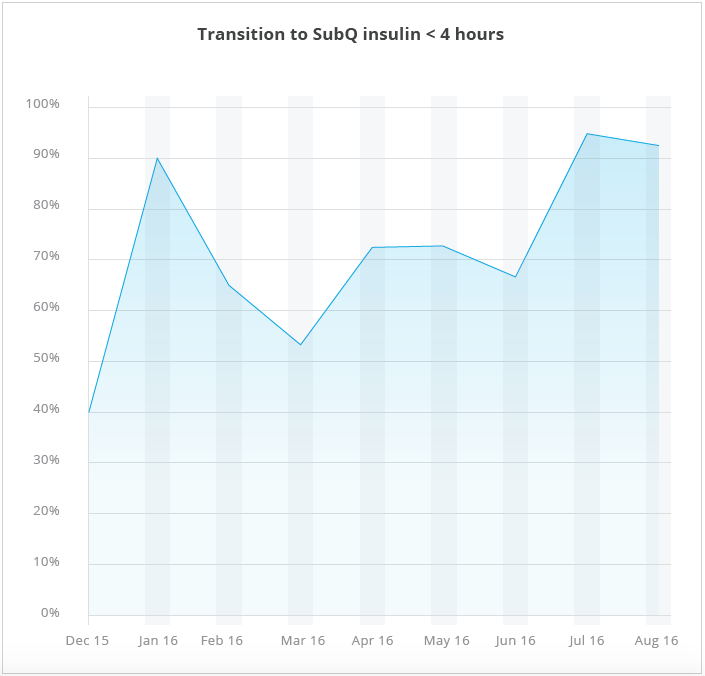
Quick transition to subcutaneous insulin: Transitioning from intravenous (IV) to subcutaneous (SubQ) in the hospitalized patient is a key step in patient care. To facilitate safe transition to SubQ insulin within four hours of medical readiness, the team developed a protocol which allows the registered nurse to transition the patient when the patient meets the pre-defined criteria, reducing potential delays in care.
Length of stay: Variation in treatment of patients with DKA had resulted in variable LOS for those patients. Therefore, the team set goals focused on improving LOS by reducing variation and inefficiencies in care for patients admitted with DKA to compete with national benchmarks at peer institutions.
Timeliness of follow-up after hospital discharge: Ensuring a smooth transition to the next care setting (most often home) is an important part of effective inpatient care. During the inpatient stay, the patients and their families are supported by the CDNs, social work, financial counselors, dieticians, certified diabetic educators (CDEs), and standard education curriculum, which helps patients feel well prepared to continue their care after discharge from the hospital. Each patient receives a comprehensive discharge plan, which outlines the expected plan of care and instructions for glucose management following discharge. To support the transition to management in the home environment, the Inpatient CPT partners with the clinic to make certain that newly diagnosed patients receive follow-up via the phone or an appointment within two weeks of discharge and a second follow-up as a scheduled appointment within a month of discharge.
With analytics, a dedicated Inpatient Diabetes CPT, and measurable goals in place, Texas Children’s has made significant strides in improving diabetes care, especially for patients with DKA. Major results to date include the following:
Currently, 94 percent of patients with diabetes receive their care in the DCU and nearly 80 percent are under the expert supervision of a CDN. Creation of a specialty unit staffed by CDNs has resulted in a highly supportive environment for patients with DKA and their families, as reflected in the patient satisfaction scores. CDNs receive standard, evidence-based education to assure competency and consistency in the treatment and education of patients with diabetes, and receive continuing nursing education through monthly educational offerings. Clinicians document patient education in the EHR, giving everyone involved in the patient’s care visibility into what education has been completed during the patient’s admission. Texas Children’s believes these educational materials could become an international standard and benefit patients worldwide.
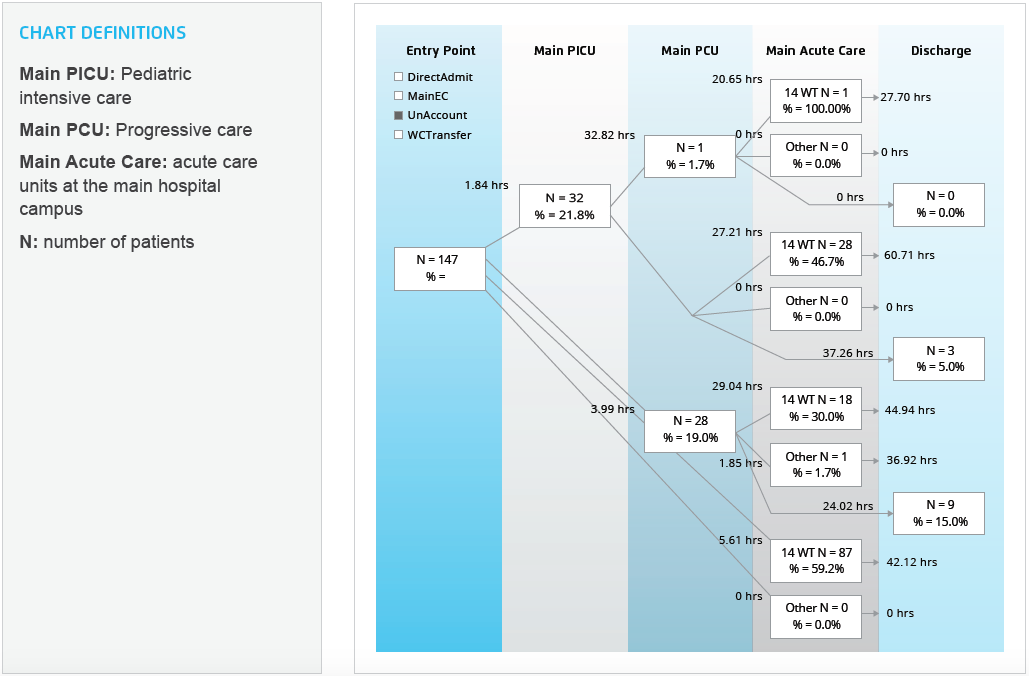
Rather than relying on manual chart review to monitor patient flow, the Inpatient CPT is able to use the pediatric diabetes analytics application to track the number of patients admitted from the emergency care center to the PICU, to the progressive care unit (PCU), to the acute care/DCU, and through the rest of their hospital stay. This easy to access visual includes patient counts and length of time in hours, from the point of entry into Texas Children’s to discharge (see Figure 1), and helps to facilitate effective bed utilization and registered nurse staffing.
As just one example of improved order set utilization, 96 percent of diabetes patients at Texas Children’s EC now receive the appropriate evidence-based evaluation (a relative increase of 17 percent and absolute increase of 14 percent). The health system has successfully carried this rate over into the DCU environment. The team attributes much of this success to the fact that the evidence-based order sets and plans of care have been well received by clinicians. The team put considerable effort into obtaining stakeholder input in the development of the order sets and protocols and spent considerable time educating clinicians who were not involved in the development as to how and why the team developed the protocols. Stakeholder input from a variety of services helped to ensure the order sets and protocols were useful for all services.
Today, 72 percent of patients with DKA receive the appropriate dose of IV insulin within one hour of it being ordered. This increased from 59 percent in FY2013 to 70 percent in FY2015, representing a relative increase of 19 percent and absolute increase of 11 percent. Despite the difficulty of changing processes in complex environments like the EC, data from the pediatrics diabetes application reveals that Texas Children’s has been successful in sustaining this improvement.
The criteria based order set has resulted in more than 90 percent of patients successfully transitioning to SubQ insulin within four hours of medical readiness (see Figure 2).
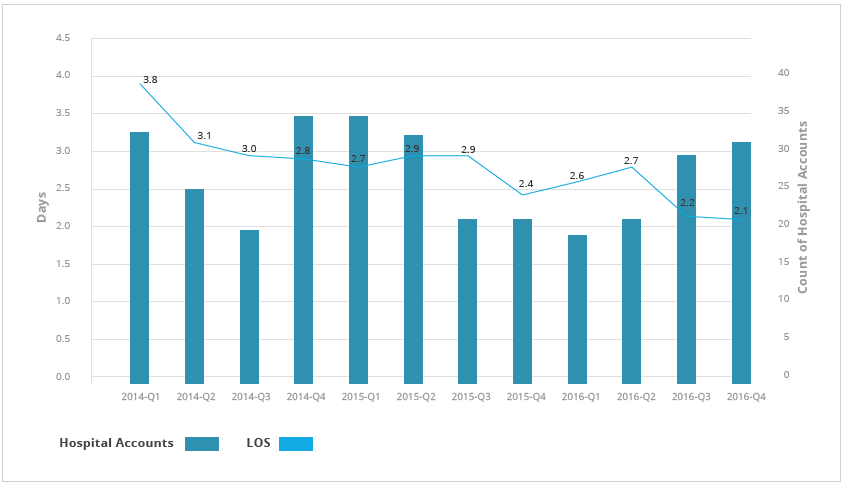
LOS for new inpatient encounters who received care in the EC from triage to discharge has decreased from 3.8 days to 2.1 days, a 44 percent relative decrease in LOS for type 1 and type 2 diabetes (see Figure 3). LOS reductions can be attributed to the reduction in the variation of care, including rapid identification of patients experiencing DKA, reducing inefficiencies of care, and the use of evidence-based order sets.
“Before we formed the DCU, we had diabetes patients going to a variety of areas within the inpatient space staffed by clinicians with varying levels of diabetes training. By developing a diabetes center of excellence, we ensure that patients receive education and management by the same group of highly trained providers in a consistent, individualized, patient-centric manner.”
– Rhonda Wolfe, RN, Assistant Clinical Director of Nursing, Texas Children’s Hospital
Texas Children’s Inpatient CPT is continuing to monitor the gains from their previous improvement work, sustain the gains and momentum of the Inpatient CPT, while also identifying new opportunities for improvement. Next, the team plans to focus their attention on improvements in care for patients with type 2 diabetes and patients who have had multiple admissions to the hospital during the year.




