Chronic diseases affect 133 million Americans, or 45 percent of the population, account for 70 percent of annual deaths—totaling over 1.7 million—and drive 86 percent of healthcare costs. Mass General Brigham (formerly Partners HealthCare), an integrated delivery system, has developed an integrated care management program (iCMP) to better manage chronic patients and treatment costs. Led by nurse care managers who collaborate with primary care providers, the iCMP has shown effectiveness in managing patients and achieving financial success, particularly during its Pilot Phase as a Medicare Demonstration Project.
One hundred thirty-three million Americans, 45 percent of the population, have at least one chronic disease. Chronic diseases are responsible for 7 of 10 deaths each year, killing more than 1.7 million Americans annually. Moreover, chronic disease accounts for 86 percent of our nation’s healthcare costs.
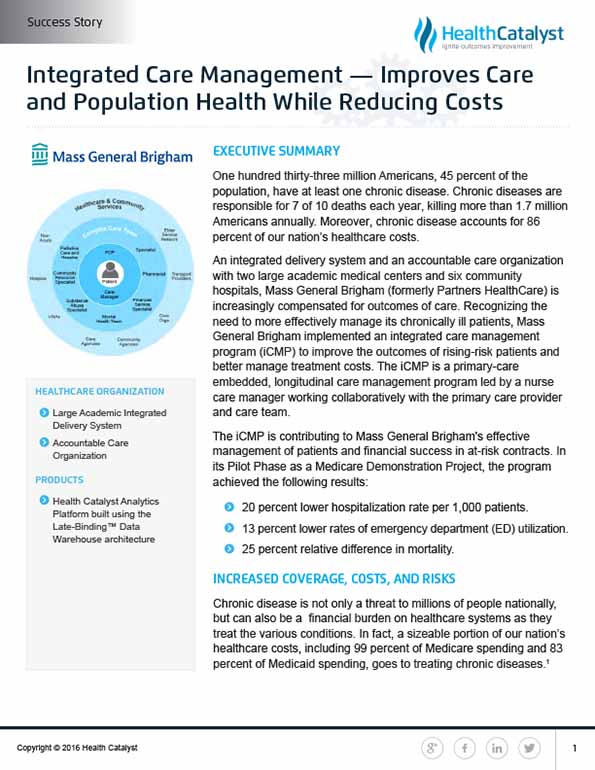
An integrated delivery system and an accountable care organization with two large academic medical centers and six community hospitals, Mass General Brigham (formerly Partners HealthCare) is increasingly compensated for outcomes of care. Recognizing the need to more effectively manage its chronically ill patients, Mass General Brigham implemented an integrated care management program (iCMP) to improve the outcomes of rising-risk patients and better manage treatment costs. The iCMP is a primary-care embedded, longitudinal care management program led by a nurse care manager working collaboratively with the primary care provider and care team.
The iCMP is contributing to Mass General Brigham's effective management of patients and financial success in at-risk contracts. In its Pilot Phase as a Medicare Demonstration Project, the program achieved significant results.
Chronic disease is not only a threat to millions of people nationally, but can also be a financial burden on healthcare systems as they treat the various conditions. In fact, a sizeable portion of our nation’s healthcare costs, including 99 percent of Medicare spending and 83 percent of Medicaid spending, goes to treating chronic diseases.1
Although healthcare organizations around the country are searching for ways to contain costs, the mission is particularly critical in Massachusetts, where cost containment legislation has restricted inflation in medical costs to 3.6 percent. Under state law, inflation of healthcare costs may not exceed the growth in wages, requiring that providers become more responsible for healthcare costs. What’s more, Massachusetts has led the nation in health reform and now has a 98 percent coverage rate.2 With the expansion of insurance, cost of care becomes an issue.
Through its ACO, which covers approximately 500,000 lives, Mass General Brigham has embraced population health management and is committed to finding better strategies, such as an iCMP for containing costs and improving care outcomes.
To ensure ongoing financial viability and success in at-risk contracting, Mass General Brigham's overall challenge is to reduce the cost of care while improving patient outcomes. Mass General Brigham's Division of Population Health Management is responsible for the organizational accountable care strategy and infrastructure.
Mass General Brigham recognized that the area of greatest opportunity for containing costs and improving care was with their adult patients who have chronic illnesses but who have not yet progressed to the point where they are incredibly complex medically. Once patients’ chronic illnesses progress to this point, they become high utilizers of high-cost services.
Mass General Brigham also identified that patients who have multiple chronic conditions often find it difficult to navigate the complex health system. Existing care models are disease- or specialty-specific, creating confusion and inadvertent fragmentation of care. Mass General Brigham recognized that it needed to better coordinate care for these patients.
If Mass General Brigham could more effectively manage the care of patients who are not yet “too sick,” it could then improve patient health and decrease cost, as care would be shifted away from high-cost inpatient hospital services and provided in lower-cost outpatient settings instead. Patients with rising risk presented the greatest opportunity for overcoming the value challenge.
Mass General Brigham needed collaboration between clinical expertise and technology to identify those patients with chronic illnesses who had the potential to become high users of high-cost services.
To more effectively manage its medically complex/high-risk patients, Mass General Brigham developed the iCMP, and embedded it within the primary care practice to integrate care along the continuum. The iCMP is led by a nurse care manager who collaborates with the patient’s primary care provider (PCP) and care team.
Patients in the iCMP receive access to specialized resources, including mental health services, community resource expertise, pharmacy, and palliative care. Support is designed to occur throughout the continuum of care, including home visits, telemonitoring, and integration with post-acute and specialty services. Patients also receive health coaching and build skill in self-management through shared decision making with the care team.
Each care manager and their team manages a mix of low-, medium-, and high-risk patients, with approximately 200 patients assigned to each team. The care managers assess patient risks and needs. They follow the patient, assessing gaps in understanding or ability to comply with the established medical treatment plan. The care managers also act as liaisons, coordinating care between providers and services, facilitating better communication and transitions.
A precursor to the iCMP included only patients enrolled in Medicare, Medicaid, or at-risk contracts. Following the development of infrastructure and technology to support the iCMP, Mass General Brigham now takes a payer agnostic approach to care management.
Effective, accurate identification of rising-risk patients is critical to effective care management. Without appropriate identification of rising-risk patients, clinicians and staff would not have the ability to engage the patient in participating in the iCMP.
To identify rising-risk patients who may be appropriate for the iCMP, Mass General Brigham needed to review clinical, operational, and financial data. Mass General Brigham used the Health Catalyst Analytics Platform built using the Late-Binding™ Data Warehouse architecture (EDW) to integrate its data. To identify patients who may be candidates for the iCMP, Mass General Brigham applies claims data from the EDW into a risk predictive modeling software. The risk software generates a list of patients who are likely to be at a higher risk for rising/high costs in the succeeding 12 months.
Also using data from the EDW, Mass General Brigham is able to compare the outcomes and cost for iCMP patients against comparison groups, enabling Mass General Brigham to demonstrate the return on investment (ROI) and outcomes of the iCMP.
The list of candidates for the iCMP is reviewed by the PCP and nurse case manager, who assess each patient’s needs and discuss additional qualitative information that may not be adequately represented within the claims data. Together, the PCP and nurse select patients who are appropriate for the iCMP.
While the care managers focus on ensuring availability of appropriate care for patients who may need additional community resources or mental health support, they also identify other, atypical areas where support is needed.
One example of this is a patient, who was being supported by an iCMP care manager, who had regular monthly appointments with her PCP to treat her venous stasis ulcers, a type of wound that develops as a result of decreased blood return to the heart. Each month, the PCP would direct the patient to wear her compression stockings, which are designed to help increase blood flow back to the heart. Unfortunately, this patient did not wear the stockings as directed, and each month the PCP would restate the importance of wearing the stockings, expressing concern about the patient’s ulcers and sharing how the stockings would help improve the current ulcer and prevent additional ulcers from developing. The patient’s ulcers were not going to get better unless she wore the compression stockings.
The care manager noticed that the patient only wore red clothing from head to toe. The care manager was certain that the reason the patient would not wear the compression stockings was because they were not red. Upon bringing this discovery to the PCP’s attention, the care manager obtained red compression stockings. The patient immediately began wearing her new, red compression stockings and her problem with venous stasis ulcers was eliminated.
Through the EDW, analytics platform, and care managers who are skilled at assessing and meeting patient needs, Mass General Brigham is able to gain valuable insight about patients who are candidates for the iCMP, as well as plan cost-effective care to best meet the patients’ needs.
Analytics supports both strategic decision making and the operations of the iCMP. IT systems improve care coordination, leveraging real-time data from the EHR. For example, when an iCMP patient is registered in the EHR for care in the ED or for an inpatient bed, an automated page goes out to the patient’s PCP and iCMP care manager for the patient. Additionally, flags noted in the EHR identify iCMP patients, helping to ensure the care team is aware of the additional care team members involved in the patients’ care who should be contacted when the patient presents to the ED or is admitted to the hospital.
The iCMP has provided positive clinical outcomes and financial benefits for at-risk contracts. Claims data from the EDW applied in the risk modeling software has resulted in the identification of more than 50,000 at-risk patients. Approximately 14,000 patients actively participate in the iCMP.
In its Pilot Phase as a Medicare Demonstration Project, when compared to a similarly selected control population, the program achieved the following results:
While the financial savings are impressive, communication among care team members has also increased, as have physician, staff, and patient satisfaction. Physicians have stated that they have better work-life balance and are satisfied they are able to focus on the most effective medical management of the patient, while other team members use their skills to help patients overcome social, behavioral, and informational barriers to care.
“Our fundamental belief is that care management is critical in population health management.”
- Sreekanth Chaguturu, MD, Vice President of Population Health Management
As part of the broader population management strategy, Mass General Brigham has expanded the iCMP systemwide and is broadening efforts, offering the program to pediatric patients
Mass General Brigham is also considering enhancements to their care management model, moving to a triad model that expands leadership to include a social worker and community health worker who would each manage cohorts of patients that would benefit the most from their specific expertise.
Mass General Brigham is also continuing to expand and improve population health and redesign primary care practices to make them more efficient and a better experience for patients and care team members. By the end of 2018, all Mass General Brigham primary care practices will receive Patient-Centered Medical Home certification.