Low back pain (LBP) is a costly issue in the U.S., exceeding $100 billion annually. Allina Health established the Spine Institute in 2011 to enhance LBP care through standardized practices. The program has successfully reduced hospital length of stay by 16 percent, post-op complications by 3.6 percent, and projected savings of $2.7 million.
Low back pain (LBP) is a common and expensive problem. The annual cost to patients, employers, and insurers collectively exceeds $100 billion in the United States, the majority stemming from lost wages and productivity.1 Indeed, LBP is one of the most frequent reasons for missed work. It is also the chief symptom driving visits to orthopedic surgeons and neurosurgeons, and the second leading symptom for visits to primary care physicians.2 As for treating the condition, there are marked variations in spinal surgery internationally and between regions in the United States.3 Outcomes can even vary within a well-respected and large delivery network.
Allina Health, a not-for-profit health care system dedicated to the prevention and treatment of illness in communities throughout Minnesota and western Wisconsin, has been recognized by many organizations for its efforts to improve the quality and safety of healthcare. In 2010, the health system noted a poor grade for spine surgery performance at some of its facilities in publicly reported data. This shone a light on a number of challenges—and ultimately prompted a major performance improvement initiative.
Allina concluded that they did not have the necessary information at hand to determine if the rating they received was accurate. Although the health system did have a data warehouse, it contained data too limited to truly understand spine care performance across the enterprise. That said, analysis of what data was there indicated significant variation in outcomes, including length-of-stay (LOS), post-operative complication rates, readmissions and costs.
Physicians lacked visibility to these variations, and of their own performance relative to their peers. Some physicians were also unaware that performance data was being collected from entities like Centers for Medicaid and Medicare Services, insurers and regulatory agencies. Nevertheless, physicians recognized and supported the need for more coordinated care of patients with LBP. They also understood the overall need to provide care at a lower cost and only provide treatment that was appropriate for the patient.
Taking measure of these current realities, Allina embarked on a sweeping initiative to transform the treatment of spine care into an integrated, multidisciplinary and evidence-based approach.
In 2011, Allina created a spine program to deliver care that supports the IHI Triple Aim in the treatment of spine disorders and LBP.4 All clinical disciplines involved in spine care are part of the program, including surgeons, physiatrists, nurses, physical therapy, social workers, and other medical spine specialists. Because spine care is a complicated and specialized area, surgeons and clinicians play key roles in designing consistently superior treatment. Value is the ultimate goal, and defined as value = (quality/cost) X appropriateness.
The Allina Health Spine Program governance structure consists of an executive committee, steering committee, and medical and surgical spine quality councils. The latter are made up of clinicians, managers, and data analysts, who identify areas of focus to improve care and outcomes. An emphasis is placed on working in close collaboration with patients to set and achieve goals for their treatment.
Clinicians follow a spine care model designed to be evidence- based, multi-disciplinary and coordinated (see Appendix A). The model strives to assure every spine patient is triaged to the most appropriate level of care, at the right time, to achieve the best possible outcome. A triaged care management system with similar characteristics has also been developed for patients with low back pain (see Appendix B).
In association with these models, the Spine Program developed standard guidelines of care. This was paired with a concerted effort to educate clinicians regarding the importance of using data, the existence of variation and how to follow an evidence-based approach based on the care model. To enable the analysis of current performance and spur clinical transformation, Allina implemented a late-binding enterprise data warehouse platform (EDW) from Health Catalyst. The EDW aggregates clinical, financial, operational, experience, and other data to create consistent views of data that informs decisions.
The Spine Program also continuously monitors clinical and patient satisfaction outcomes throughout the care delivery continuum— including patients cared for at independent physician clinics, Allina’s Hospitals and the Twin Cities Spine Center. Great attention is directed toward increasing patients’ quality of life, including their functional abilities as well as lowering perceived pain levels. To that end, Allina deployed a Spine Advanced Application. This is an analytics solution that monitors and manages LOS, readmissions, and provider preventable conditions (see Figures 1-3).
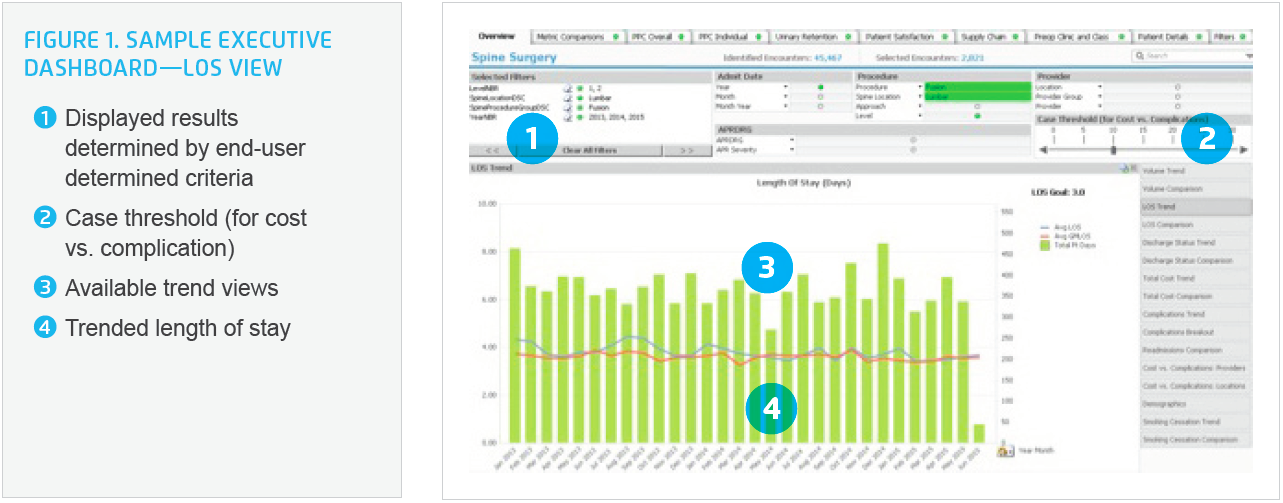
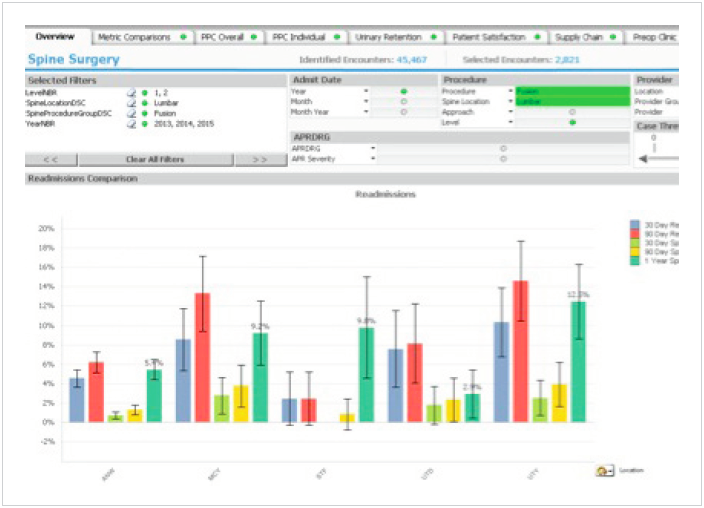

The insights gleaned from the dashboard are highly useful to drive behavior change in an effort to improve performance and outcomes. Physicians were shown their data relative to their peers to help inform and engage in the improvement initiatives. As an incentive to share data and adhere to care guidelines and models, spine specialists are given access to Allina’s large primary care physician referral base.
Allina has implemented a successful, collaborative spine care coordination program. Much of this success is due to the direct involvement of care providers in designing and leading the program. Their work is sustained by an effective decision support and analytic infrastructure that monitors outcomes and manages the care of spine patients. This also gives Allina’s care providers access to good data. Here are just some of the key results:
16 percent reduction in LOS. LOS dropped from an average of 4.26 days in 2012 to 3.6 days in the first quarter of 2015, a 16 percent improvement.
3.6 percent reduction in post-op complications. The overall rate of provider preventable post-operative complications (e.g., post- surgical infections, hemorrhage, pulmonary edema, respiratory failure, renal failure, etc.) dropped from an average of approximately 9 percent in early 2014 to an average of approximately 5.8 percent in early 2015.
Projected $2.7 million savings achieved with supplies standardization. After some physicians could not show the implant they used improved care, and other physicians had worse outcomes with the implant they were using, a consensus-driven effort to streamline the use of implants (from 27 implant vendors to only 6) led to major implant savings.
The availability of data played a notable role in driving consensus on this decision. It has also helped motivate and engage providers to drive out inappropriate variation and promote standardization.
This expands beyond supplies to include standardization of the care model and best practices protocols. For example, a “fusion risk score” has been developed by surgeons at Twin Cities Spine Center that provides a simple and consistent method of assessing perioperative risk.
In a telling indication of the success of adopting consistent standards in spine care, Allina has realized a significantly higher percentage of medical versus surgical care for lower back pain.
“Having access to detailed data helped us better understand the complexities of spine care and the key drivers of outcomes.”
– Amir Mehbod, MD, Chair, Spine Surgical Council
Allina continues to develop a highly integrated, multidisciplinary and patient-centric approach to patients with spine issues. Specific next steps include the broad introduction of the fusion risk score and measuring the financial impact of the spine program. With such notable results from improving spinal care, Allina plans to expand integrated, coordinated care to more clinical service lines. It is clear this is an effective approach to improving care for patients and providing their physicians with quality data.
The Allina Spine Institute spine coordinated care model
The Allina Spine Institute spine coordinated care management system for LBP


