In the U.S., one in three pregnant women give birth via cesarean section, exceeding WHO recommendations. MultiCare sought to standardize care to enhance women's health services, improve patient outcomes, and maintain market share by launching a Women’s Collaborative focused on improving clinical care and patient outcomes for women’s services systemwide.
One in three pregnant women give birth via cesarean section in the United States, which is more than double the rate the World Health Organization (WHO) recommends. And instead of decreasing, the overall C-section rate in Washington State increased 73 percent from 1996 to 2009. C-section rates are just one area of women’s care where our practice in the U.S. lags behind the science and knowledge of best practice. MultiCare Health System believes that all of its female patients should experience the same high-quality care across its integrated delivery system. The health of the next generation depends on it.
MultiCare recognized that it had to standardize care across its system to meet quality standards, improve its patients’ experiences and outcomes, and maintain its market share. The health system launched a Women’s Collaborative, the sole purpose of which was to improve clinical care and patient outcomes for women’s services systemwide.
In the United States, 32.7 percent of pregnant women give birth via cesarean section—more than double the rate the WHO recommends.1 Instead of decreasing, the overall C-section rate in Washington State increased 73 percent from 1996 to 2009.2 Increases in primary C-sections where there is no indicated risk have been attributed to changes in obstetric practice rather than changes in the medical risk profile.3 Rates for vaginal birth after C-section are low. Once a woman undergoes a C-section, it is highly likely that subsequent births will also be via C-section.4 Decreasing the rate of unnecessary C-sections, especially for first-time mothers, is therefore an important goal for healthcare providers like MultiCare, an integrated delivery system in the state of Washington. But C-section rates are just one area of women’s care where practice in the U. S. lags behind the science and growing knowledge about best practice.
MultiCare is a growing system—it acquired Auburn Medical Center (AMC) in October of 2012. National research findings indicate that hospital mergers tend to decrease the quality of patient care.5 MultiCare’s leaders were determined to grow market share while at the same time improving the quality of care the organization provided to patients. Following the AMC merger, they saw an opportunity to improve the quality of the health system’s obstetrical and gynecological (OB/GYN) services.
To address these patient care concerns, MultiCare formed a Women’s Collaborative. Collaboratives—part of MultiCare’s highly developed approach to quality improvement—consist of multidisciplinary groups of clinicians and support staff whose sole purpose is to improve clinical care and patient outcomes for a defined population across all of the health system’s sites of care.
MultiCare faced considerable challenges as it embarked on its journey to improve maternal care while simultaneously integrating AMC into the system. This initiative marked the first time MultiCare had attempted a project of this magnitude—combining birthing facilities at three different hospitals with different cultures and care approaches into one large group, with aligned best practices.
At the point of acquisition, the birthing center at AMC had seen a reduction in deliveries from 75 to 30 per month; AMC had lost many experienced staff and was suffering from low morale. Improving OB/GYN performance at AMC and across the system would require systemwide standardization of best practices. MultiCare leaders recognized, however, that implementing standard practice across hospitals with unique cultures could meet significant resistance from clinicians. Implementing best practices would mean asking a wide range of OB/GYN practitioners—including community, employed, and affiliated physicians—to change the way they had done their work for many years. Building relationships would therefore be essential to the success of the initiative.
Standardizing best practice would also necessitate data to uncover opportunities for improvement, as well as an infrastructure for measuring progress. Previous experience indicated to health system leaders that analytics was essential to provide feedback on performance—in aggregate and by individual practitioner—in order to drive and sustain significant gains. However, MultiCare had identified problems in reporting and source data for maternal health patients, which had resulted in a low level of trust in the validity of the data.
The Women’s Collaborative was launched in January, 2013 to establish a systemwide forum to standardize maternal care, improve clinical outcomes, reduce variation, and decrease costs. An external consultant identified concerns with performance on clinical indicators in publicly reported data at all facilities—and particularly at AMC—that could potentially affect future contract negotiations with payers. In response to these findings, and in the interest of improving patient care, MultiCare charged the Women’s Collaborative with the following tasks:
The following outlines the solutions MultiCare put in place to accomplish these objectives.
The Women’s Collaborative wasted no time in putting structures in place to smooth the transition to standardized care based on best practices. Within one month, the Collaborative had established regular, systemwide meetings and weekly OB workgroup meetings, including one for AMC to track and monitor implementation of operational and clinical care improvements. The intent of these meetings was to improve women’s services across the organization while providing additional support to bring the newly acquired AMC into the effort.
Another priority for the Collaborative’s leaders was recruiting physician champions at each facility. A leadership team, including these physician champions, met weekly to keep the work moving forward.
The detailed work of the Collaborative was performed in smaller groups, called workgroups, each focused on improving a specific care process. The leadership team provided oversight and removed barriers to these workgroups’ progress.
The initial workgroups within the Collaborative focused on improving the following care processes:
In setting up the Collaborative and rolling out its improvements, a culture of engagement proved a key driver for success. Rather than imposing new practices on clinicians, the Collaborative sought and encouraged clinician input throughout the process. This engagement empowered clinicians to make decisions about practice and process that would improve patient outcomes and experience. The high volume of participation among physicians created powerful momentum for change motivated by the desire to improve care.
As the initiative gained momentum, the Women’s Collaborative expanded its focus. Late in 2013, it began to participate in multiple statewide initiatives related to perinatal care. This deliberate strategy involved participation of a MultiCare representative in the perinatal partnerships organized under the governor, the HealthCare Authority, the Department of Health, WSHA, and the March of Dimes. MultiCare’s leaders recognized that those participating in such initiatives would influence statewide policy and felt a duty to share the health system’s hard-earned expertise on these important topics. These statewide programs, as well as national quality improvement programs, led the Women’s Collaborative to focus its efforts on improving these areas:
Successful deployment of culture and practice changes on the scale that the Women’s Collaborative was pursuing required a common vision across the three hospitals and complete integration of the new hospital (AMC) into the MultiCare system.
From experience with previous Collaboratives, MultiCare leaders knew that standardization of practice would only be effective when executed well. The following were key areas of focus for the Women’s Collaborative to ensure a high level of adoption and buy-in among clinicians:
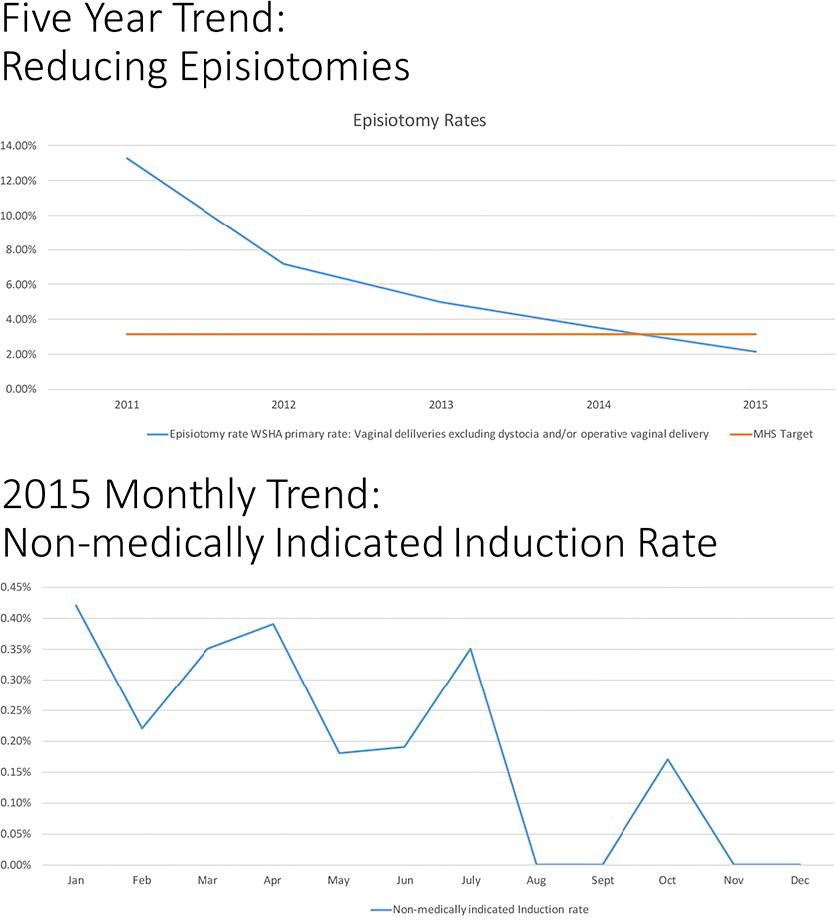
From its experience in other Collaboratives, MultiCare recognized the impact that reliable analytics and a team-focused dashboard could play in accelerating quality improvement (see Figure 1). The Collaborative used a Late-Binding Data Warehouse Platform and analytics applications from Health Catalyst to support practice changes, provide feedback to clinicians on their performance, and to identify which interventions were effective.
Because of concerns about data integrity, the Women’s Collaborative had to validate the data sources and clean up the reporting stream before implementing an analytics application and dashboard. Validating the data required an auditing process that took a year to complete. Physicians actively participated in this process, which engendered their eventual acceptance and championship of the data. Once the data was accepted, the Collaborative created structured electronic notes to standardize clinical documentation, and it was able to put the analytics application in place quickly with a high level of acceptance.
The Collaborative formally standardized practice and defined metrics to measure performance, then used analytics to show improvement and compare results among the facilities and individual practitioners. Collaborative leaders knew that transparency and healthy competition could be an effective motivator. In fact, it was clear that AMC was successfully integrated when its clinicians became the leader in MultiCare on some of the key quality metrics. With high levels of clinician engagement and trust in the data, the Women’s Collaborative soon found itself in a conundrum caused by its own success: It had identified more opportunities for improvement than the health system could support with available analytics resources. (MultiCare dedicates a set amount of analytics support to each Collaborative.) The Women’s Collaborative therefore had to prioritize workgroups and projects and identify in what order each would receive analytic resources. In some cases, the Collaborative instructed its workgroups to start on other aspects of their improvement work—such as developing practice guidelines and pathways, aligning policies and procedures, and laying the groundwork for deployment—before they received analytics support and dashboards to monitor performance.
The Women’s Collaborative has contributed to organizational performance and generated many impressive results for MultiCare.
Whereas at the beginning of the initiative, clear guidelines for diagnosing labor arrest requiring C-section delivery did not exist, MultiCare’s implementation of evidence-based guidelines and standards resulted in further reduction of its NTSV C-section rate. It is 9 percent less than the national average and continues to improve. MultiCare has already reached and exceeded the national 2022 goal of less than 23.9 percent.
After normalizing data to include AMC in the baseline, MultiCare achieved a six-point increase in market share for inpatient OB/GYN services between 2012 and 2014 (the latest market data available). In fact, MultiCare is the market leader for outpatient services for Women and Neonatology in Washington’s Pierce and South King counties and has increased its number of deliveries by 21 percent since 2013.
This increase in market share resulted from the effective integration of AMC into the MultiCare system, brought about in part by its active participation in the Women’s Collaborative and the improvements in patient care and outcomes for OB/GYN services systemwide.
The Women’s Collaborative drove significant, measurable improvements in multiple areas of care delivery, including the following:
The Collaborative’s efforts also delivered a measurable reduction in length of stay (LOS):
"Team-focused dashboards are powerful. We discovered quickly that presenting data in dashboards plays an important role in engaging clinicians to change the way they deliver care. Changing practice is hard—some physicians have been practicing the same way for decades! The data allowed us to show them that the practices they were used to didn’t necessarily produce better outcomes. As a physician, when you can see that you’re the outlier on the bell curve of performance, you start to ask yourself what you’re doing differently from your peers, and then you make changes.”
– Stephen Poore, MD, Medical Director, MMA Women’s Health
The highly functioning Women’s Collaborative continues to make progress at great speed. Team members are constantly identifying new opportunities for improvement. They plan to maintain their high level of participation in statewide and national improvement efforts, sharing their expertise while influencing public policy.
Some of the workgroups that started under the Women’s Collaborative have evolved to become programs in their own right. As such, they will be run through operations rather than continue as part of the Collaborative. Examples of such workgroups are the chemical dependency initiative and the high BMI program for pregnant women. Both of these efforts have received statewide recognition for their innovative approach to treating high-risk and underserved populations.
Other workgroups will continue to operate under the Women’s Collaborative. A promising new workgroup is focused on achieving the perfect hysterectomy and is already demonstrating improved patient outcomes. These and other improvements spurred by the Collaborative continue to be influential in negotiations as MultiCare enters into risk-based contracts. Health system leaders have no doubt that the engagement and teamwork exemplified by the Women’s Collaborative are a powerful force for improving patient care and outcomes.




