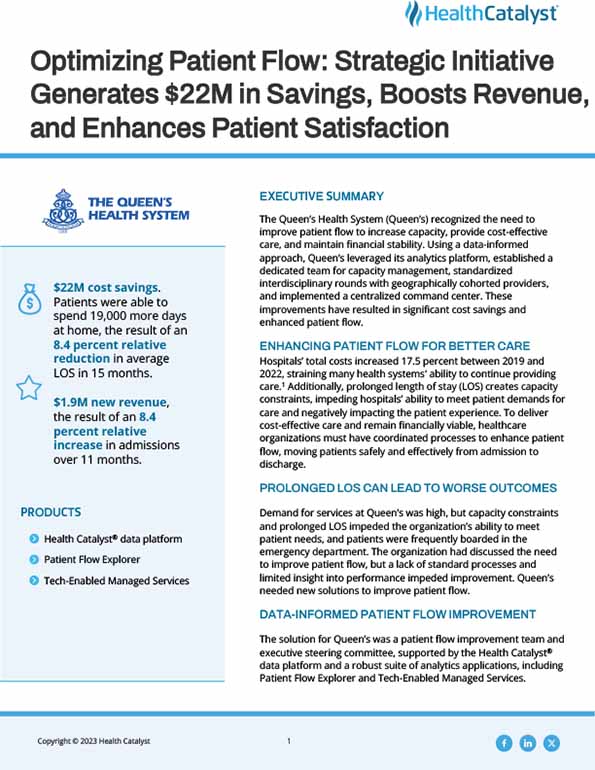
The Queen’s Health System (Queen’s) recognized the need to improve patient flow to increase capacity, provide cost-effective care, and maintain financial stability. Using a data-informed approach, Queen’s leveraged its analytics platform, established a dedicated team for capacity management, standardized interdisciplinary rounds with geographically cohorted providers, and implemented a centralized command center. These improvements have resulted in significant cost savings and enhanced patient flow.
Hospitals’ total costs increased 17.5 percent between 2019 and 2022, straining many health systems' ability to continue providing care.1 Additionally, prolonged length of stay (LOS) creates capacity constraints, impeding hospitals’ ability to meet patient demands for care and negatively impacting the patient experience. To deliver cost-effective care and remain financially viable, healthcare organizations must have coordinated processes to enhance patient flow, moving patients safely and effectively from admission to discharge.
Demand for services at Queen’s was high, but capacity constraints and prolonged LOS impeded the organization’s ability to meet patient needs, and patients were frequently boarded in the emergency department. The organization had discussed the need to improve patient flow, but a lack of standard processes and limited insight into performance impeded improvement. Queen’s needed new solutions to improve patient flow.
The solution for Queen’s was a patient flow improvement team and executive steering committee, supported by the Health Catalyst® data platform and a robust suite of analytics applications, including Patient Flow Explorer, and Tech-Enabled Managed Services.
The patient flow improvement team and executive steering committee clarified roles, responsibilities, and decision-making authority, making changes in three key areas, and engaging all team members to improve patient flow.
Additionally, Queen’s leverages the Patient Flow Explorer analytics accelerator to:
Health Catalyst Tech-Enabled Managed Services support ongoing clinical quality improvement, advancing analytics adoption, and facilitating improvement using a seven-step improvement model, giving Queen’s team members a proven methodology to drive improvement.
Queen’s data-informed improvement efforts are producing meaningful results. The organization has improved capacity management effectiveness, decreased LOS, increased the ability of the organization to serve more patients, and improved the patient experience. Results include:
"By leveraging our data and analytics, we’ve been able to significantly improve patient flow—reducing length of stay, decreasing costs, and increasing revenue—all leading to enhanced healthcare delivery and an improved patient experience."
- Matthew Ing, MD, VP of Medical Affairs & Chief Medical Officer, The Queen’s Medical Center
Queen’s plans to expand its standard interventions across the health system and will continue to use data, analytics, and the proven improvement methodology to further improve patient flow, ensuring patients can access care when they need it. Queen’s is also building a centralized command center to further expand its patient flow efforts.