Every year, almost 51,000 patients die from pneumonia with pneumonia ranking as the fourth leading cause of death for the elderly. After implementing a pneumonia care pathway and analytics application, Piedmont Healthcare reduced its pneumonia mortality rate.
Patients with pneumonia account for over 400 thousand emergency room visits, nearly 1.1 million inpatient hospitalizations, and more than 5.7 million inpatient days each year in the U.S. Every year, almost 51,000 patients die from pneumonia. Among the elderly, community-acquired pneumonia is an increasing problem, now ranking as the fourth leading cause of death.
Piedmont Healthcare, a not-for-profit integrated health system serving Georgia, had multiple order sets for disease management, but the health system lacked a uniform care pathway for the treatment of pneumonia. Care provided for the treatment of pneumonia was often not in alignment with evidence-based guidelines, such as antibiotic selections. This lack of consistency increased both LOS and cost, and a lack of case-specific data made the development of a uniform best practice for pneumonia treatment challenging. By accessing detailed case data with the help of analytics, Piedmont was able to identify and develop best practices for the treatment of pneumonia, driving out the variation that increased costs and reduced the overall quality of care.
Each year in the U.S., patients with pneumonia account for over 400 thousand emergency room visits, nearly 1.1 million inpatient hospitalizations, and more than 5.7 million inpatient days—resulting in almost 51,000 deaths a year as a result of pneumonia. Community-acquired pneumonia is an increasing problem among the elderly, with pneumonia-associated deaths ranking fourth in leading causes of death in elderly people.1,2
The Infectious Diseases Society of America (IDSA) and the American Thoracic Society developed a unified community-acquired pneumonia guideline intended primarily for use by emergency medicine physicians, hospitalists, and primary care practitioners. However, the extensive literature evaluation suggests the guidelines are also an appropriate starting point for consultation by specialists.3
As part of a sweeping initiative to improve clinical outcomes for patients with pneumonia, the Centers for Medicare and Medicaid Services and Hospital Quality Alliance began publicly reporting 30-day readmission rates and pneumonia mortality measures, implementing penalty programs for hospitals performing poorly on these metrics.4
Piedmont Healthcare is a private, not-for-profit organization with 11 hospitals, 24 urgent care centers, 555 clinic locations, and more than 2,000 clinic members, serving nearly 2 million patients across Georgia. Founded over 100 years ago, Piedmont is transforming healthcare, creating a destination healthcare system known for the best clinicians and a one-of-a-kind experience that always puts patients first.
As part of its ongoing efforts to improve quality, Piedmont sought to identify opportunities to improve the care provided to patients with pneumonia. While Piedmont had some pneumonia performance data, it lacked the comprehensive data needed for performance improvement. Piedmont was not able to easily monitor the number of patients with pneumonia, making it difficult to evaluate variations in care. Evaluating the impact of specific interventions on performance was even more challenging, making targeted improvement activities difficult to accomplish.
Piedmont had multiple order sets for disease management. However, it lacked a pneumonia specific care pathway, resulting in large variations in best practices for care. Often, care provided was not in alignment with evidence-based guidelines, such as antibiotic selections, and nursing care was inconsistent and lacked uniformity. This lack of consistency increased both LOS and cost.
Piedmont identified that, in order to improve the quality of care provided to its patients with pneumonia, it needed better data and analytics that would enable it to monitor the impact of practice changes on patient outcomes, while driving out the variation that increased costs.
To improve the care provided to patients with pneumonia, Piedmont established an inter-professional pneumonia clinical standardization committee comprised of healthcare professionals representing all facets of pneumonia care across the entire system. The committee is charged with facilitating a culture of evidence-based practice throughout the organization using a data-driven approach to continuous improvement. The goal of the pneumonia clinical standardization committee is to use evidence-based practice to improve the care provided to patients, reduce LOS, reduce cost per case, improve mortality, and improve the readmission rate.
Membership for the clinical standardization committee includes an internal medicine physician champion from one of Piedmont’s rural hospital locations, pulmonologists, emergency department physicians, infectious disease physicians, members of the nursing leadership team, case managers, respiratory therapists, pharmacists, IT staff, and quality improvement professionals. Membership selection was broad and purposeful, in an effort to encourage collaboration, build trust, and engage diversity of content knowledge.
Piedmont supports the clinical standardization committee in its improvement efforts by providing a dedicated dyad of improvement specialists. The improvement specialists have either operational or clinical knowledge in addition to the performance improvement skills needed to facilitate effective improvement efforts. With this support, the committee developed an evidence-based pneumonia care pathway based upon IDSA guidelines. The pneumonia care pathway serves as an educational and reference document, defining pneumonia standard work for key care phases including:
Standard order sets were developed using the latest guidelines. The order sets were built within the EMR providing the foundation for clinical standardization for the following populations:
All order sets include standard nursing interventions that are pre-selected. The antibiotic options are in alignment with IDSA guidelines and based upon severity of illness and are in alignment with national sepsis guidelines and Piedmont’s sepsis order sets. Key guiding principles used to develop the order sets include ensuring they are:
To ensure widespread adoption of the pneumonia care pathway and order sets, Piedmont developed a comprehensive communication plan outlining pre-implementation, implementation, and post-implementation activities.
To improve Piedmont’s ability to use a data-driven approach to improvement, the organization leveraged the Health Catalyst® Analytics Platform and broad suite of analytics applications, implementing a pneumonia analytics application that provides comprehensive data about its performance (see Figure 1).
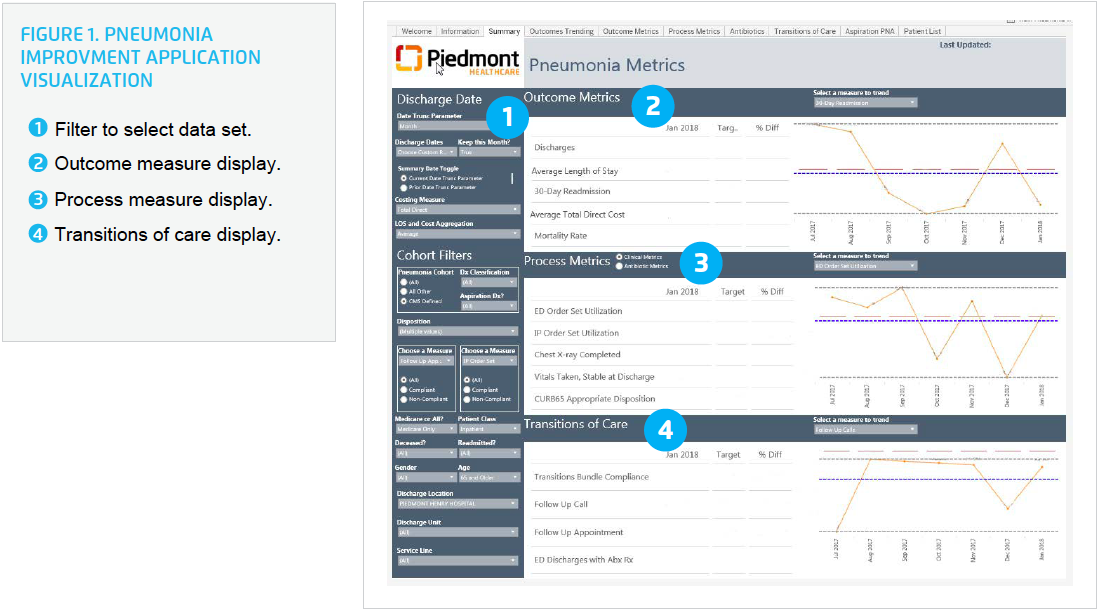
The analytics application helps Piedmont drive efforts to reduce pneumonia mortality and improve pneumonia-associated LOS, readmission rates, and cost per case. The analytics application focuses on providing data to improve initial triage/disposition of patients with pneumonia, antimicrobial selection and timing, and risk stratification for care transition planning.
For the first time, Piedmont is able to evaluate the impact of order set utilization on patient outcomes and give providers their specific performance data, demonstrating to them the impact of their care decisions on their patient’s outcomes. For example, using the analytics application Piedmont is able to review antibiotic selection and is able to compare the effectiveness of the selected antibiotics, and other components of the order set, on patient mortality and LOS.
Having detailed, actionable data enables the pneumonia clinical standardization committee leaders to have personalized coaching discussions with providers who are resistant to adopt the new care pathway and order sets. Sharing data demonstrating patient outcomes when using the order sets has been powerful, helping Piedmont gain provider buy-in of the pneumonia care pathway and order sets.
To improve the use of data and analytics to drive improvement, Piedmont increased the number of people with access to the analytics application, allowing clinicians independent access to the dashboard to view their care pathway, order set utilization, and outcomes of their patients.
Care management clinicians access the analytics application, using it to identify patients with pneumonia who are still in the hospital. Care managers help ensure the correct order set is ordered. Prior to the patient being discharge from the hospital, care managers facilitate timely follow-up appointments with the appropriate provider and complete follow-up phone calls to smooth care transitions.
In less than one year, using this collaborative data-driven approach, Piedmont has achieved dramatic improvements in the outcomes for patients with pneumonia, including:
The key to this success was the use of the provider-specific data and the impact of the evidence-based order set on patient outcomes. This approach contributed to Piedmont exceeding its goal for systemwide order set utilization in just six months.
“Being able to tie specific improvement activities to patient outcomes is very powerful. As frequent users of the order sets we impact quality scores—but more importantly we positively impact our patient’s outcomes.”
– Dr. Andy Jaffal, MD, MMM, CPE, Chief Hospitalist, Piedmont Healthcare
Piedmont is committed to maintaining a continuous quality improvement program dedicated to providing the highest standard of care for patients diagnosed with pneumonia. Piedmont uses quarterly pneumonia clinical standardization committee meetings to ensure it sustains the gains and further improves the pneumonia care pathway and order sets. Piedmont plans to spread these best practices to its emergency department and ambulatory care clinics.


