Over 30 million Americans have diabetes, with many undiagnosed. Hypertension affects a third of adults, often unnoticed, leading to significant healthcare costs. The Queen’s Health Systems adopted Self-Service Analytics to implement custom algorithms from the Hawaii Department of Health to better identify and improve the management of patients with diabetes and hypertension.
More than 30 million Americans have diabetes, and nearly a quarter of those patients have yet to be diagnosed. A third of American adults have hypertension (HT) and many do not know they have it as the condition often has no signs or symptoms. Together, diabetes and HT account for $285.6 billion in healthcare costs. Undiagnosed diabetes and HT can lead to significant additional diabetes-related complications and an increased risk of heart disease and stroke.
The Queen’s Health Systems (QHS) needed to implement custom algorithms developed by the Hawaii Department of Health (DOH) to better identify patients with undiagnosed pre-diabetes, diabetes, and hypertension, as well as patients with past-due diabetes/pre-diabetes screenings. Although QHS staff was capable of building and implementing the algorithms, staffing constraints and disparate EMRs created delays and challenges. QHS needed to dramatically accelerate the process in order to secure a DOH grant designated for improving the management of patients with diabetes and HT.
To meet these challenges, QHS adopted the Self-Service Analytics Suite, enabling the accelerated implementation of the custom algorithms.
Approximately 30.3 million American adults have diabetes. Of those, 23.1 million are diagnosed, while 7.2 million go undiagnosed. In the U.S., diabetes remains the 7th leading cause of death and costs more than $237 billion annually.1
Type 1 diabetes is usually diagnosed at the onset of symptoms, but type 2 diabetes often goes undiagnosed until after complications, such as kidney damage, nerve damage, or other heart and blood vessel disease have already developed.
The same is true for hypertension (HT). HT is of particular concern because it increases the risk of heart disease and stroke, the leading causes of death in the U.S. Typically, HT has no warning signs or symptoms, and many patients are unaware they have it.2 Yet, one in three U.S. adults do, costing the nation $48.6 billion each year. Early diagnosis and treatment of diabetes and HT reduce long-term diabetes-related complications and the risk of early HT-related morbidity and mortality.
QHS is the largest nonprofit network of hospitals and health-related entities serving the people of Hawaii. U.S. News & World Report ranks QHS as one of the top 50 hospitals for diabetes and endocrinology specialties. The Queen’s Clinically Integrated Physician Network (QCIPN), with more than 1,100 providers on five islands, is a collaboration between QHS, community physicians, and physician organizations. QHS and QCIPN looked to improve its identification process for these at-risk patient populations so that these unidentified and undiagnosed conditions can be treated.
QHS and QCIPN had identified diabetes and HT prevention and management as a primary community health need when QCIPN was approached by the DOH and Mountain-Pacific Quality Health regarding the availability of grant funds intended to improve the management of patients with diabetes and HT.
The grant funds were available to support the implementation of algorithms developed by the epidemiology team at the DOH that would enable the identification of patients with pre-diabetes, patients who appeared to have diabetes but who had not yet been diagnosed, and patients with undiagnosed HT.
Identifying patients who have not yet been diagnosed is challenging because relevant clinical information is documented in multiple places in the EMR making manual identification a burdensome, labor-intensive process. Additionally, because of how data is stored in the EMR, patients who have not yet been diagnosed are often “hidden.” The algorithms were designed to automate identification, decreasing manual work and enhancing providers’ ability to effectively manage patients.
Previously, QCIPN had attempted to use claims data to identify patients and develop a similar list, but the aged data was not helpful to providers. Often, when the patient list was brought to the practices, the providers would share that they were already aware of the problem. Other times, patients on the list had changed practices or passed away. Providers needed more timely data to proactively engage with patients.
While the algorithms held promise, integrating them into the EMR presented some substantial challenges. The EMR’s registry starter sets were difficult to customize. It was possible to develop a registry that could “slice and dice” patient data effectively but doing so would take months or even a year to build. QHS employees had the skills to build and implement the algorithms, but the organization needed to execute quickly to meet the grant requirements. The EMR team’s staffing constraints further limited the organization’s ability to meet the deadline.
Even more challenging was that QCIPN providers use more than 30 disparate EMRs. Using the EMR to implement the algorithms could present a problem in the future, and could result in an incomplete picture of the patient, and an inaccurate patient list, limiting the organization’s ability to proactively engage patients and reduce early morbidity and mortality.
The organization needed a solution that could quickly integrate the algorithms to accurately identify patients with pre-diabetes, patients who appeared to have diabetes but who had not yet been formally diagnosed, and patients with undiagnosed HT.
Given the limitations of the EMR, QHS and QCIPN leadership suggested the team use the Health Catalyst® Data Operating System (DOS™) Platform, and the associated Self-Service Analytics Suite to implement the custom algorithms.
DOS combines the features of data warehousing, clinical data repositories, and health information exchanges in a single, common-sense technology platform. The analytics platform is able to integrate clinical, financial, and operational data from multiple source systems across QHS and QCIPN.
QHS and QCIPN formed a workgroup to develop and implement the custom algorithms. The team included epidemiologists from the DOH, IT staff, project managers, EMR experts, data experts, informaticists, Health Catalyst analysts and professional services, and clinicians.
The team met weekly over the course of several months, working to understand the intent of each algorithm and determining the best method for implementing it. Ultimately, the team decided to integrate the custom algorithms into the Pop Analyzer™ analytics application.
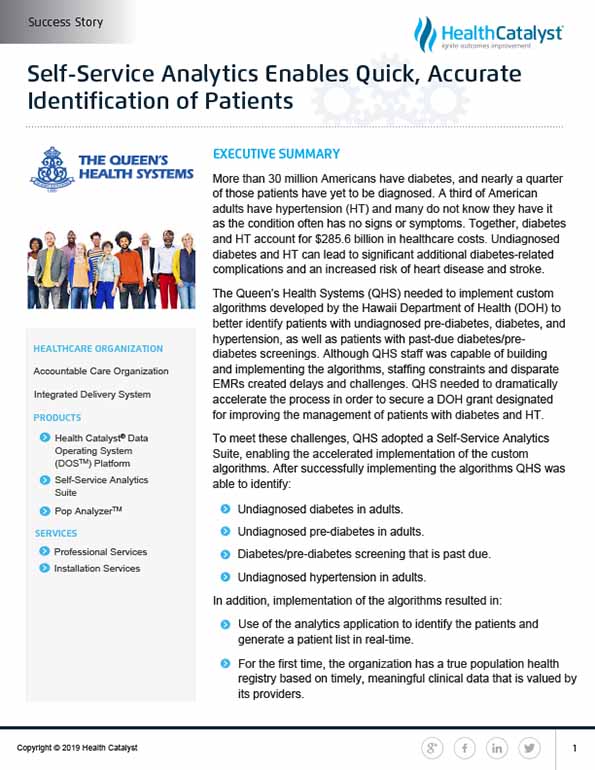
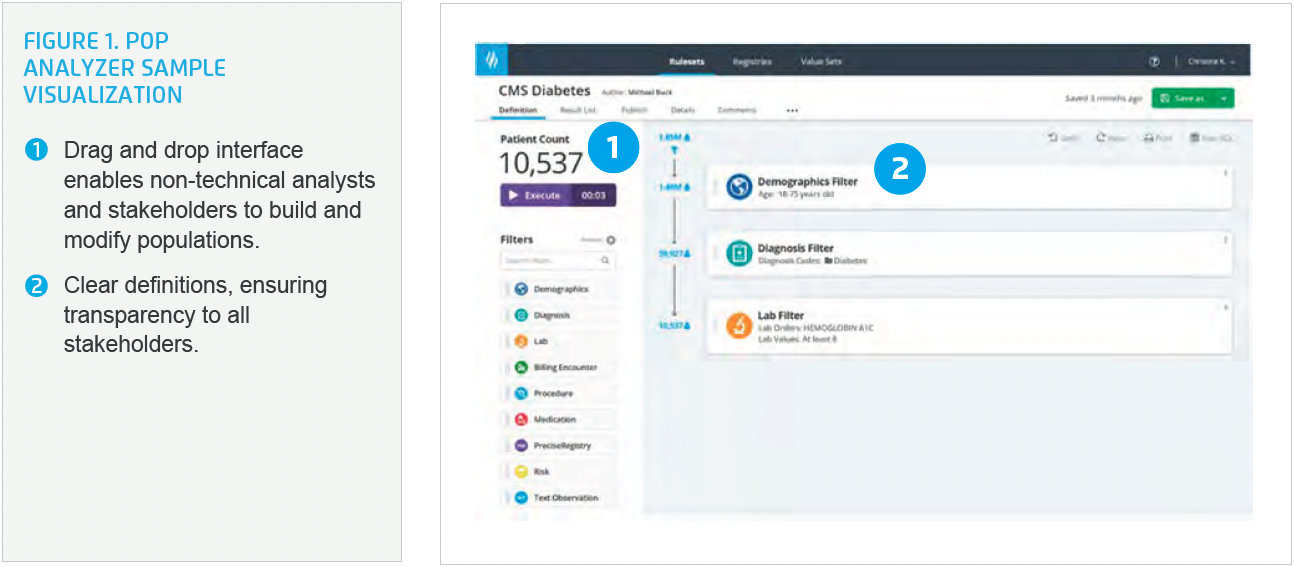
Pop Analyzer, an application within the Self-Service Analytics Suite, enables users to dynamically author, manage, view, and publish pre-built and custom population ruleset definitions using an elegant drag-and-drop interface (see Figure 1). These rulesets can be published as registries and augmented with summary metrics using Health Catalyst tools. The Pop Analyzer library includes access to 400 nationally recognized populations, as well as national quality improvement and regulatory code sets to build accurate populations faster (see Figure 2).
The team also identified and validated the data required to effectively implement the custom algorithms and accurately identify patients. They configured the analytics application to bring in the appropriate data and accurately identify the patient cohorts.
By demonstrating its ability to use the Self-Service Analytics Suite to accurately and quickly identify patients, QHS and QCIPN met the DOH requirements and was able to secure grant funds to implement and integrate the custom algorithms into the analytics application.
QHS and QCIPN subsequently implemented algorithms that identify:
QHS is now able to deliver aggregate reporting for clinical quality measures CMS 122 and CMS 165, and aggregate numerator and denominator reporting. It is also able to provide a de-identified data extract for the patient population meeting the algorithm criteria, improving understanding of the local population’s health status and informing investment in future programs to improve population health.
Using the analytics application, QCIPN was able to easily and effectively identify patients with pre-diabetes, patients with diabetes who had not yet been diagnosed, and patients with HT who had not yet been diagnosed. Previously these patients were “hidden” in the EMR and could not be identified.
The team was able to use the analytics application to identify the patients and generate a patient list in real-time during the team’s standing weekly meeting. For the first time, the organization has a true population health registry based on timely, meaningful clinical data that is valued by its providers.
“Health Catalyst has demonstrated the value of data analytics in the clinical setting. EMRs are not built to perform the type of analytics we need to improve the health of populations.”
– Mia Taylor, MSN, FNP-BC, APRN-RX, Director, Community & Post-Acute Care Services, The Queen’s Health Systems
QHS and QCIPN plan to integrate the output of the algorithms into its care coordination analytics application and use the information from the analytics application to improve the decision support for providers. Integration of the patient list into the workflow will enable care coordinators to review the data, and support providers’ ability to proactively engage with patients to improve early management of diabetes and HT. This will advance the effectiveness of its population health programs, improve the health of the community, and reduce early morbidity and mortality.