Healthcare-associated conditions (HACs) remain prevalent despite being preventable. Implementing best-practice bundles effectively reduces HACs, but monitoring compliance can be burdensome. Texas Children's Hospital has streamlined reporting to quickly identify at-risk patients, track clinician adherence to these bundles, and reduce manual chart reviews for calculating HAC rates.
Texas Children’s Hospital is committed to providing the highest-quality care possible for children and families. It has fully embraced a culture of safety, quality and transparency. In fact, the health system shares publicly its performance on multiple nationally recognized quality and safety measures, including adverse drug events, hand hygiene and Central Line-Associated Blood Stream Infection (CLABSI) rates.1
Reducing the rate of healthcare associated conditions (HACs)—such as CLABSI, surgical site infections (SSIs), respiratory viral infections and others—has always been important to Texas Children’s, an organization consistently ranked among the top children’s hospitals in the nation. This priority has become even more pressing as the Centers for Medicare and Medicaid (CMS) and other payers begin to tie reimbursement to performance against HAC quality benchmarks. Although pediatrics has largely been excluded from this trend, forward-thinking organizations are working to improve care delivery by tackling the problem of HACs in children.
Rates, symptoms and interventions for many HACs differ markedly between children and adults,2 so the established evidence-based treatments for adults are not always appropriate for children. At the same time, few pediatric-specific prevention standards are available because very little research on HACs in children has been performed. This situation creates a significant challenge for health systems like Texas Children’s seeking to implement best practices to prevent HACs in a pediatric setting.
In 2012, Texas Children’s joined the Solutions for Patient Safety National Children’s Network to participate in a program to develop and validate pediatric safety standards and benchmarks. This collaborative—which now includes more than 80 children’s hospitals—has established evidence-based care delivery bundles for many HACs and continues to work on the rest. The collaborative shares best practices, benchmarks against one another and learns from each other’s successes.
In February, 2015, the Solutions for Patient Safety National Children’s Network revealed impressive results reducing HACs in children. Since 2012, the network collectively saved 2,500 children from serious harm, translating to more than $60 million in savings. The implementation of best-practice bundles—validated by network participants—is the driving factor behind these results. For example, the SSI bundle drove a 19 percent SSI reduction across the network as of May 2014.3
Although the children’s hospital community has made great strides in developing and implementing best-practice bundles, tracking providers’ compliance with these bundles can present a significant challenge. At Texas Children’s, it is critical to track not only HAC rates but also whether clinicians are complying with best practices.
However, collecting data to inform both the HAC rates and bundle compliance rates at Texas Children’s was a time consuming process. The following are two examples of the amount of effort required to gather this data:
The team expended similar effort to track other hospital-acquired infections. Then, on top of that, they would spend additional time each month aggregating the data across the health system’s units for enterprise-wide reporting.
Another challenge the quality and safety team faced was a lack of timely data. Waiting for the ICD-9 coding to come through post- discharge meant the HAC rates had a 30-day delay. Physicians and leadership did not know until the end of the month where they stood with their HAC rates. Because of this data delay, it was often too late to intervene while the patient was still in the hospital. If, for example, a patient had a hospital stay of several months and developed a VTE at some point during that stay, that patient wouldn’t show up on the team’s HAC list until after discharge.
Finally, the infection control team faced the challenge of outdated software. They stored all the HAC data they had manually aggregated into their infection control database. However, this infection surveillance system was more than 15 years old and no longer supported by the vendor. The team urgently needed to replace the system with a new a data-entry, tracking and analytics solution.
Texas Children’s had implemented a late-binding data warehouse platform (EDW) by Health Catalyst to drive multiple performance improvement initiatives. Their EDW aggregates clinical, financial, operational and other data to create a consistent view of the data—a single source of truth to inform decisions. On top of the EDW, the health system implemented an advanced analytics application from Health Catalyst to serve as their infectious disease surveillance system. The team is beginning to capture confirmed infection cases in the EDW platform, which, over time, will enable them to completely phase out the use of their antiquated infection surveillance system.
The Regulatory Explorer analytics application enables Texas Children’s to easily track and analyze—and prevent—the incidence of a variety of HACs in near real-time. For example, the application’s CLABSI module displays the number of patients with a central line on any given day. The drill-down feature enables the director for infection control to look at patient-level data for CLABSI and enact a near real-time intervention if a central line has been in the patient for 15 days or more (see Figure 1).
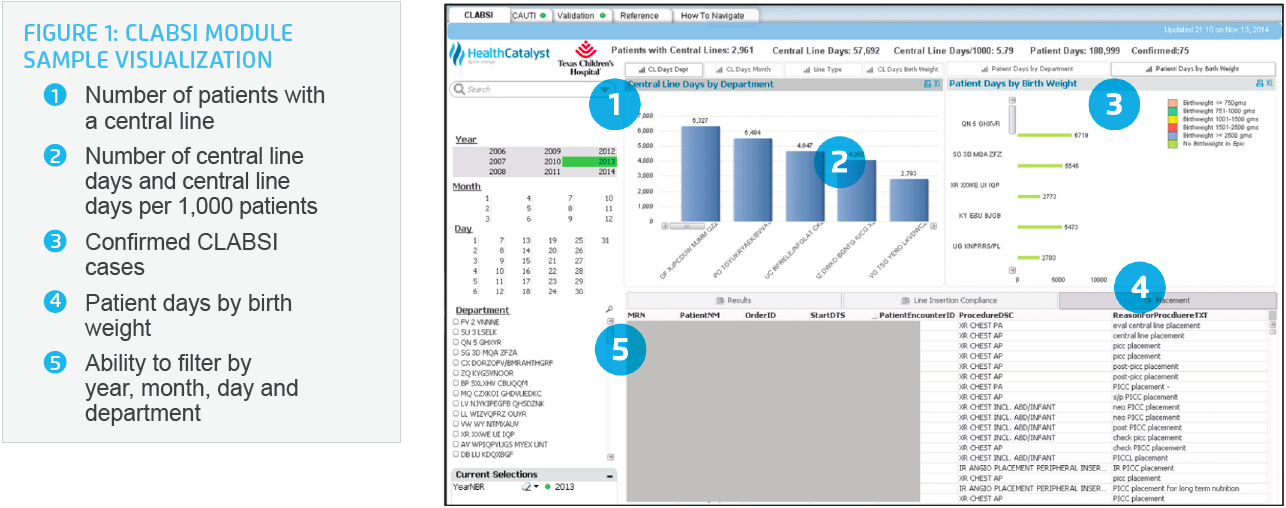
The application delivers similar visualizations for Catheter Associated Urinary Tract Infection (CAUTI) and Ventilator Associated Pneumonia (VAP) that track urinary catheter days and ventilator days, respectively.
The application’s SSI module enables users to track the number of surgeries by type and the number of SSIs (see Figure 2).
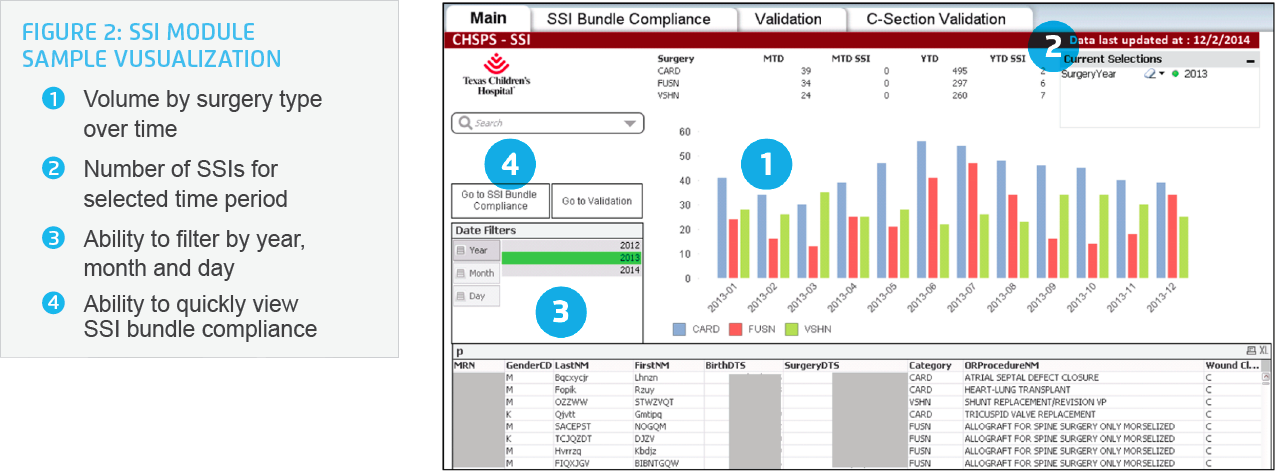
Not only can the team view high-level performance on SSIs, they can also drill down to the best-practice bundle elements and to the individual patient level. By drilling down, the team can identify which best practices are being implemented, which are not and which patients were affected. For example, the team can now see antibiotic timing (minutes between the antibiotic administration and incision, as well as re-dosing) and identify compliance with that element. They can also begin to investigate the clinical implications of compliance with that element and of variations in the timing of the dose.
The flexibility of the application, in combination with clinical oversight, allows the team to proactively address HACs. It serves as a surveillance tool that complies with the Center for Disease Control’s National Healthcare Safety Network definitions while simultaneously allowing the team to track best practices specific to pediatrics. They can quickly access near real-time data and intervene to address new clinical problems as they arise.
Texas Children’s has experienced tremendous success in identifying evidence-based bundles to reduce HACs in children through their partnership with the Solutions for Patient Safety National Children’s Network. Using the EDW and analytics applications to identify vulnerable patients and monitor clinicians’ compliance with best-practice bundles, the health system has achieved the following:
"Thanks to Health Catalyst, our infection control team has experienced a shift from a data-collection mindset to a quality- improvement mindset. The analytics solution decreases the amount of manual data collection the team has to routinely perform, so they can focus instead on what’s important. And it gives us near real-time data so that we can act to improve care immediately.”
– Elaine Whaley Director of Infection Control Texas Children’s Hospital
As the Regulatory Explorer analytics application supporting patient safety rolls out more broadly across the enterprise, leaders from 20 departments throughout Texas Children’s will be able to visualize their infection rates at any given point in time rather than relying on the infection control team. Soon, the antiquated infection surveillance system will be replaced entirely by the new application. In addition, with the roll out of additional best-practice bundles and dashboards, they will be able to view rates and bundle compliance for more HACs, driving a further reduction in HAC rates.
The health system will also maintain its participation in the Solutions for Patient Safety National Children’s Network. This collaborative will continue to assess evidence for appropriate pediatric-specific guidelines. Its 2015-2016 goals are as follows:
Texas Children’s expects the cost of care to the patient will decrease as further complications necessitating multiple follow-up appointments—and even readmission—are prevented by consistent use of appropriate best practices.