Allina Health sought to reduce 30-day potentially preventable readmissions (PPRs) by enhancing follow-up care. The organization utilized predictive analytics, redesigned care processes, and engaged patients and families to improve outcomes. Its comprehensive approach has led to significant improvements in clinical and financial results.
Nearly 20 percent of elderly patients released from a hospital are readmitted within 30 days.1 Readmissions are becoming an issue health systems have to manage to improve quality of care and avoid Medicare penalties imposed on hospitals with excessive re-hospitalizations.
Allina Health—a 13-hospital health system serving Minnesota and Wisconsin—believes that patients deserve to receive optimum follow-up care and support after discharge from the hospital, thus minimizing readmissions. Allina Health decided to focus on 30-day potentially preventable readmissions (PPRs) as its global outcome measurement. PPRs are determined based on the clinical relationship of the readmission to the prior discharge.
Software provided by 3M Health Information Systems (HIS) derive the clinical relationships between hospitalizations that determine PPRs. Allina Health built analytic capabilities using the PPR data outputs to identify opportunities for improvement in care coordination at discharge and to test quality improvement ideas.
Allina Health’s multipronged solution to reducing PPRs included redesigning care processes, implementing predictive analytics to identify at-risk patients, using analytics to measure the impact of its interventions, and educating patients, families, and clinicians.
Allina Health’s efforts are driving measurable improvements in clinical and financial outcomes.
Far too often, patients discharged from U.S. hospitals are subsequently readmitted for the same condition. In fact, almost 20 percent of elderly patients released from a hospital return within 30 days, and more than one third return within 90 days.2 Such readmissions not only negatively affect patients’ health but also cost the nation billions of dollars.3
Traditionally, efforts to reduce readmissions focused on hospitals, but today’s industry is aware that many factors along the care continuum influence readmissions. In fact, the main culprit behind avoidable readmissions is a fragmented system that does not transition patients smoothly from the hospital to appropriate followup care. Without care management, patients are often confused about discharge instructions, taking medications properly, or getting needed follow-up care.
The reducing avoidable readmissions effectively (RARE) campaign decided to tackle the readmission problem in the state of Minnesota by focusing on those re-hospitalizations deemed preventable.4 To do so, RARE used the clinical relationships identified by the 3M HIS software to create statewide Minnesota PPR reports. Allina Health benchmarked their hospitals compared to others in the state and noted opportunity for overall PPR reduction. Allina Health proactively brought the software in house and began looking at PPR outcomes to drive improvement.
Aware of its PPR outcomes, Allina Health—a not-for-profit healthcare system comprised of 26,000 employees, 5,000 affiliated and employed physicians, 13 hospitals, 90 clinics, 16 pharmacies, and numerous specialty medical services—is redesigning its processes to more effectively manage care transitions at the time of discharge. By ensuring patients receive the support they need as they transition out of the hospital, Allina Health is furthering its mission of helping people throughout Minnesota and western Wisconsin live healthier lives.
Like many health systems nationwide, Allina Health had to prepare for the potential of CMS (Centers for Medicare & Medicaid Services) penalties for poor readmission performance, as well as for the emerging pay-for-outcomes reimbursement model. To do so effectively, Allina Health’s leaders needed to understand the scope of the health system’s readmissions problem.
Allina Health turned to data analysis to shed light on its readmissions performance. Specifically, Allina Health leaders wanted to understand the health system’s performance on readmissions within the first seven days after discharge (a national analysis had demonstrated that 40 percent of clinically related readmissions occur within that period). Allina Health’s analysis revealed that during the three-month-long 2013 reporting period, 492 of its patients returned to the hospital within seven days of discharge, and 225 of those patients returned in the first four days. These statistics made it clear to health system leaders that they needed to manage care better for patients during this critical week.
However, coordinating an effort to reduce readmissions across a large health system required overcoming significant challenges. Leaders recognized that about 40 percent of Allina Health’s patients had complex discharge needs that required care management to achieve a successful transition; however, the health system did not have an effective way to identify these patients and focus the appropriate care resources on them. Complicating matters further, the information required to manage transitions was distributed across various locations in the electronic health record (EHR) and across multiple tools.
Furthermore, Allina Health’s analysis revealed an unacceptable level of variation in the case-finding process. Clinicians managing care across sites and across specialties relied on different methodologies to determine which patients should receive post-hospitalization care and support. Allina Health’s leaders recognized that this lack of standardization in case finding was likely contributing to high readmission rates.
Allina Health addressed its readmissions challenge by designing a solution that comprised four key areas:
Allina Health leaders recognized that they needed to redesign the care transition process in order to lower the risk of PPRs. They also recognized that a successful transition from the hospital required the active participation of both the patient and the care team.
Allina Health therefore undertook a system-wide redesign of hospital care management over a two-year period. The linchpin of this redesign was a new process called a Transition Conference (TC)—a facilitated meeting between a patient at risk for readmission, the care team, and other key stakeholders to outline a plan for continued care after the patient leaves the hospital. The patient, the patient’s caregiver or spokesperson, an RN care coordinator or a social worker, and the inpatient physician must attend the TC. When applicable, other care team members (such as the primary care provider, rehab providers, representatives of a skilled nursing facility, home health, pharmacists, or dietitians) also attend the meeting.
The TC process works as follows:
Allina Health leaders recognized that getting participation from physicians would be critical to the success of the TC. They strategically engaged physicians through three key actions: they included physicians in the development of the model, they identified a physician champion who carried the message of the model’s importance throughout the organization, and they incentivized physicians for their participation.
Continuous improvement of this TC process remains an important focus of Allina Health’s team. Through ongoing feedback from involved clinicians (physicians, nurses, pharmacists, social workers, and others), the team has identified a number of barriers to the TC process. These barriers included time constraints, competing resource demands, and difficulties determining appropriate handoffs for the outpatient setting. The team has been able to address and correct these issues.
With the TC process in place, Allina Health took its efforts a step further. Leaders wanted to create a model that would enable clinicians to proactively identify patients who would benefit most from a TC. They recognized that analytics and predictive models offered a cutting-edge method for identifying and stratifying patient populations into risk categories.
Therefore, Allina Health developed a predictive model for readmissions that uses data within the electronic health record (EHR) to assign a risk level to each inpatient. The model calculates a readmissions score for each patient in order to determine his or her risk level. A high-risk patient identified by Allina Health’s algorithm has a 20 percent or greater chance of having a 30-day readmission. Risk-level calculations take into account such factors as a patient’s medical history, demographic information, current clinical data, and prior utilization of the Emergency Department and inpatient services. Tests of the model demonstrated high predictive accuracy (a predictive model C-statistic of 0.729).
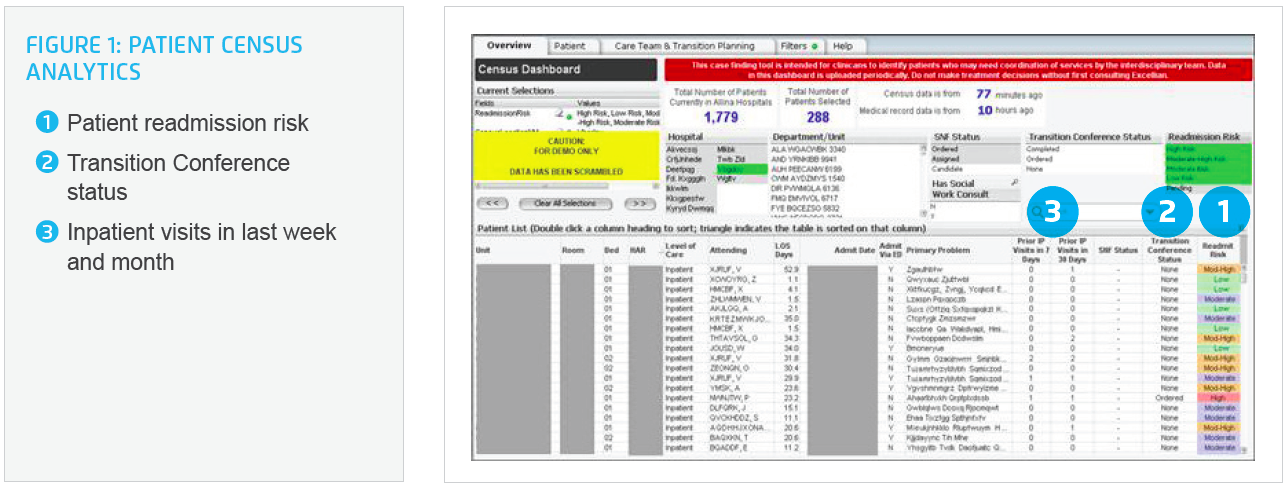
Allina Health also implemented an analytics platform built using the Late-Binding ™ Data Warehouse Architecture from Health Catalyst. Leveraging this new platform, Allina Health developed patient census analytics that enabled clinicians at the point of care to quickly identify patients who might benefit from a TC (Figure 1). Risk levels appear in the application 24-48 hours after a patient’s admission. Delivering the data to frontline caregivers in an actionable, digestible format enabled them to target the right patients for the TC process in a timely fashion. Allina Health involved frontline clinicians in designing the dashboard, thus increasing their engagement with the new system.
Analytics also enabled Allina Health to track the effectiveness of these new programs and interventions. Team members identified the key clinical variables of the patient population for which transition conferences were completed. Using third-party PPR software, they then used those variables to compare the outcomes of patients who received a TC and those who did not, thus measuring the program’s impact on readmissions within 30 days across all conditions. Allina Health then incorporated these readmissions metrics into its organization-wide scorecard.
Allina Health leaders recognized that the success of its readmissions program would depend on active engagement of patients as well as internal care teams. The organization therefore designed the TC process to educate and support patients—and to provide the same information to patients’ families or in-home caregivers. Allina Health also developed standardized and easy-to-understand materials to help educate and engage patients at the time of discharge.
Engaging care teams was an equally important component of Allina Health’s program. Therefore, program leaders assigned a team member to focus on internal marketing and raising awareness of the initiative. This individual develops materials describing the goals and key components of the program, writes a newsletter, and manages a robust intranet site (accessible across the organization) that provides program updates and houses all related materials.
Since the program’s inception in April 2012, Allina Health has completed 11,969 TCs—5,805 for high-risk patients, 4,370 for moderate-high risk patients and 1,794 for low or moderate risk patients. As a result, the health system has experienced positive results on multiple fronts.
Measurable improvements in clinical and financial outcomes include:
In the period of January – December 2015, Allina Health measured a significant reduction in PPRs for patients in all risk categories who participated in a Transition Conference. This result includes a:
In the period of January through December of 2015, Allina Health saw an impressive 27 percent relative reduction in PPRs for patients who had a follow-up appointment in a clinic within five days of discharge.
By comparing actual readmissions over the improvement period with expected readmissions for all at-risk patients, Allina Health calculated a $3.7 million reduction in variable costs. The health system attributes these savings to the new readmissions program. (Results baseline is January-December 2013)
“Predictive analytics are on the cutting edge of identifying patients at risk for a hospital readmission. It’s important to keep in mind, though, that assigning risk to patients in this innovative way won’t be effective unless we use it in a practical manner to redesign care processes.”
– Amirav Davy, Senior Clinical Data Analyst, Allina Health
Allina Health has plans in place to expand its readmissions program and hardwire the process into the care model to make it even more reliable and effective. Program leaders are also working to refine predictive analytics to improve their ability to manage at-risk populations effectively.
A particularly important initiative for the program is to integrate other sources of data into the patient census analytics application. Allina Health plans to incorporate claims data and to subsequently work more closely with payers. In addition, the team seeks to integrate patient and family data into the application, thus making it more bidirectional. The team believes that making data more meaningful and useable for patients and families will engage them to help lower readmissions even further.
1, 2. Jencks, S.F., Williams, M.V., & Coleman, E.A. (2009). Re-hospitalizations among patients in the Medicare fee-for-service program. The New England Journal of Medicine, 360(14), 1418-1428. Doi: 10.1056/NEJMsa0803563
3. Robert Wood Johnson Foundation. (2013, March). Reform in action: How the U.S. health care system can reduce avoidable readmissions.
4. Institute for Clinical Systems Improvement, the Minnesota Hospital Association, and Stratis Health. (2014, August). Reducing Avoidable Readmissions Effectively. (2016, March 21)