It is estimated that $25 to $45 billion is spent annually on avoidable complications and unnecessary hospital readmissions—the result of inadequate care coordination and insufficient management of care transitions. By implementing care coordination programs and leveraging its analytics platform, the University of Texas Medical Branch reduced its readmission rate and achieved significant cost avoidance.
Researchers estimate that in just one year, $25 to $45 billion is spent on avoidable complications and unnecessary hospital readmissions, the result of inadequate care coordination and insufficient management of care transitions.
While increasing its efforts to reduce its hospital readmission rate, the University of Texas Medical Branch (UTMB) discovered that it lacked standard discharge processes to address transitions of care, leading to a higher than desired 30-day readmission rate. To address this problem, UTMB implemented several care coordination programs, and leveraged its analytics platform and analytics applications to improve the accuracy and timeliness of data for informing decision making and monitoring performance.
Hospital readmissions are costly and can have negative consequences for patients. Readmissions totaled $7 billion in aggregate hospital costs for four high-volume conditions: acute myocardial infarction (AMI), heart failure (HF), chronic obstructive pulmonary disease (COPD), and pneumonia.1
Inadequate care coordination, including insufficiently managing care transitions, has been estimated to account for $25 to $45 billion in wasteful spending through avoidable complications and unnecessary hospital readmissions.2 To reduce readmission rates, hospitals must improve the effectiveness of transitions of care,including addressing breakdowns in communication, and improving patient education and clinician accountability.3
UTMB has a long history of advancing health sciences education, research, and patient care. It was the first academic health center in Texas and is home to the state’s first schools of medicine, nursing, and allied health sciences. For 125 years, the university has maintained a forward-thinking spirit that has enabled it to serve its students, its patients, and people in Texas and beyond in innovative ways. In keeping with this focus, UTMB searched for ways to improve care for its patients by reducing hospital readmission rates.
UTMB recognized that it had a higher than desired 30-day readmission rate that was most likely a result of its lack of standard processes for discharge and transitions of care from hospital to home. Additionally, the organization faced several challenges in lowering readmission rates that were related to information and care coordination.
For instance, UTMB lacked the necessary data to be able to identify the patients at highest risk for readmission, nor could it pinpoint the factors contributing to readmission. Patient education materials were also not standardized, resulting in variation in the information the patient received—no clear processes were in place to ensure the patient understood the materials offered. Patients were sometimes overwhelmed with complex discharge instructions, leading to medication mismanagement or an unclear understanding of what signs and symptoms indicated that they should seek care from their healthcare provider. The process for scheduling a hospital follow-up appointment varied by care unit, resulting in inconsistent discharge follow-up appointments for patients. All of these factors made it difficult for patients to do the things necessary to help themselves recover and avoid the need for additional healthcare interventions.
For the hospital and providers, obtaining accurate data on readmission rates required multiple steps. This complexity delayed the availability of data by 90 days, negatively impacting UTMB’s ability to use this information to identify potential issues and proactively make improvements.
After identifying the barriers, it faced in attempting to reduce readmissions, UTMB determined it needed to standardize its discharge processes, address transitions of care, improve access to the data and analytics required to identify opportunities for improvement, and improve the ability to monitor its effectiveness in reducing unnecessary readmissions.
UTMB established the CARE (Controlling Avoidable Readmissions Effectively) collaborative to reduce unnecessary hospital readmissions through coordination of care, improved access to primary care, behavioral healthcare, and specialty care, and improved utilization of standard processes and technology.
The multidisciplinary CARE collaborative includes a physician champion and key stakeholder participation from nurse leaders, physicians, patient care facilitators, case managers, and social workers. This group meets monthly to confirm project alignment and support, ensuring communication of project priorities, activities, and progress toward the goal of reduced readmissions. Through CARE, UTMB established standard processes for documenting patient complexity and co-morbid diagnoses, thus improving the accuracy of clinical documentation, and better communicating the patient’s medical needs.
UTMB also designed and implemented an evidence-based process for managing care transitions from the hospital to home using Project BOOST (Better Outcomes for Older Adults through Safer Transitions)—a set of interventions developed by the Society of Hospital Medicine. BOOST includes standardized tools to identify high-risk patients, educate them on their conditions and possible side effects of medication, schedule follow-up appointments, and perform medication reconciliation at discharge to make certain that drugs prescribed at discharge don’t harmfully interact with previously prescribed drugs.4
Understanding the importance of care coordination, UTMB developed the role of patient care facilitators, who coordinate the care of patients at high risk for readmission.
Discharge planning begins shortly after the patient is admitted to the hospital, using the 8P risk assessment screening tool to identify which patients have the highest risk for readmission. The 8P risk assessment is completed on the first day of admission for each new patient and is documented in the EMR. Patients with three or more of the following indicators are identified as high risk for readmission:
Patient care facilitators receive a list of patients who are at high risk for readmission each day, as well as a list of patients who have been readmitted within 30-days of discharge. This list is used for intensive rounding and case management while the patient is in the hospital, and to prioritize follow-up phone calls after discharge.
The patient care facilitators actively manage patients who are screened as high risk, entering a customizable care plan into the EMR, incorporating evidence-based practice standards. The standardized interventions include:
Recognizing the importance of confirming the patient’s understanding of the treatment plan and the effectiveness of the teach-back method on helping improve transitions of care for patients, educational offerings about the teach-back method are provided hospital-wide for providers, nurses, and care managers.
Rather than making follow-up appointments at the time of discharge, follow-up appointments are made using a centralized service within 72-hours after discharge, allowing the patient to go home and get settled prior to making the appointment. This limits the need to reschedule or inadvertently scheduling overlapping appointments and ensures the patient is scheduled with the appropriate service (primary care, behavioral health care, or specialty care).
To improve the accuracy and timeliness of data for informing decision making and monitoring performance, UTMB made the decision to use the Health Catalyst® Analytics Platform and broad suite of analytics applications, implementing the Readmission Explorer analytics application (see Figure 1).
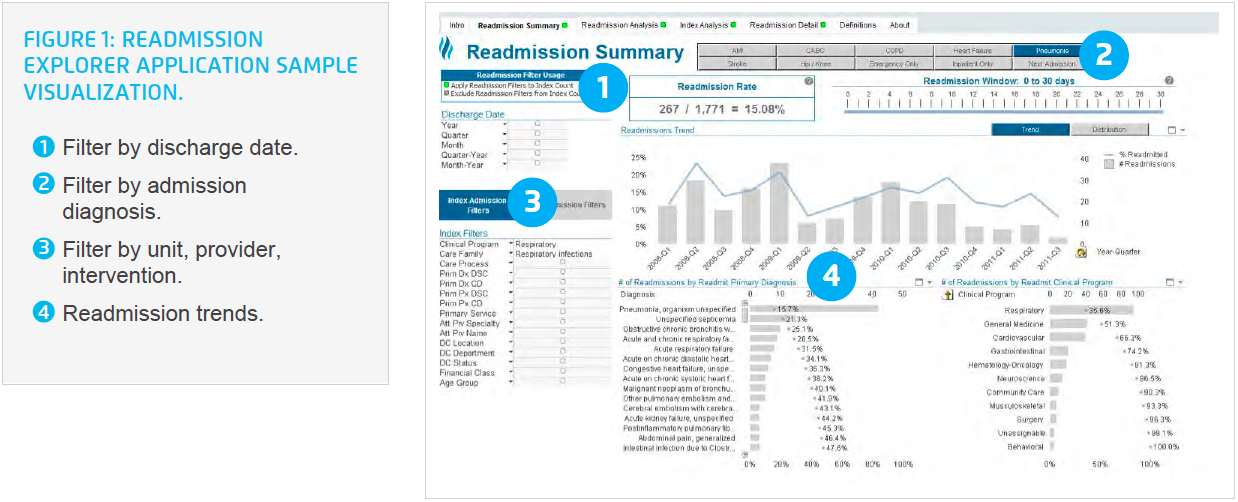
The analytics application provides UTMB visibility into a broad spectrum of readmission metrics for all-cause readmissions, unplanned readmissions, and emergency department visits. This information is updated daily, providing UTMB ready access to meaningful, actionable data.
Using the analytics application, UTMB can view data by patient demographics, discharge status, provider, and other metrics. UTMB uses the analytics application to monitor trends associated with readmissions, identify normal or special cause variation, and to pinpoint areas where transitions of care could be further improved, and unnecessary readmissions further reduced.
For example, when the data indicated that HF patients were one of the main sources for readmissions, UTMB developed collaborative relationships with outpatient care management services to develop a focused plan to facilitate smooth transitions for patients with a HF diagnosis. Supported by findings of a root cause analysis for the causes of readmissions, outpatient services provided to HF patients at high risk for readmission include transition care calls, home visits, assistance obtaining needed supplies, and continued care management services as appropriate.
The data obtained from the analytics application is also included on the organization’s balanced scorecard, used to communicate progress on 30-day all-cause readmission rate reductions, further refining processes and continuing to spread best practices across the system. In addition to using data and analytics, the CARE collaborative conducts detailed weekly root cause analyses to identify reasons for readmissions, developing action plans to address the reasons for readmission events.
UTMB implemented a comprehensive, evidence-based, multidisciplinary approach to improve transitions of care, introduced a new role to facilitate effective coordination of care for patients at risk for readmission, and utilized analytics to better inform timely decisions. Combined, these changes enhanced the transitions process and improved both the patient experience and outcomes. Using this evidence-based, data-driven approach, UTMB has made substantial improvements in the transitions of care processes, leading to impressive results:
“Using teach back and disease-specific patient education has made a real difference in the patient’s understanding of their care and has improved patient satisfaction with nursing and physician communication.”
– Brianna Salinas, MSN, RN, CNL, Patient Care Facilitator
Building on its success, UTMB continues to refine its care transitions program. Future work includes collaborating with long-term care, skilled nursing facilities, and home health providers to further refine outpatient transitions, reducing unnecessary, costly readmissions, providing the necessary care in the most appropriate care setting.