Read how UnityPoint Health leveraged information from a readiness assessment, an opportunity analysis, and expert resources, enabling the organization to establish a prioritization and implementation strategy to drive outcomes improvement and reduce clinical variation.
Reducing unnecessary clinical variation is necessary in today’s healthcare market for both clinical and financial reasons. Two major drivers for this are the shift from fee-for-service to value-based reimbursement and the need for improving clinical outcomes such as reducing complications and readmissions.
Leaders for UnityPoint Health, a healthcare system serving Iowa, western Illinois, and southern Wisconsin, recognized the importance of reducing clinical variation, and the need to have strong physician champions and robust analytics to effectively support improvement efforts. However, it also realized that without understanding organizational strengths and weaknesses related to adopting change and improving outcomes, it would struggle to successfully implement initiatives that delivered the desired benefits and sustained improvements over time. By consistently integrating information from a readiness assessment, an opportunity analysis, and expert resources, UnityPoint Health was able to establish a prioritization and implementation approach to outcomes improvement.
Reducing unnecessary clinical variation is necessary in today’s healthcare market for both clinical and financial reasons. Two major drivers for this are the shift from fee-for-service to value-based reimbursement and the need for improving clinical outcomes such as reducing complications and readmissions. It has been recognized across the U.S. that success in reducing clinical variation is highly dependent on having engaged physician champions armed with easily accessible data and analytics leading to data-driven decisions.1 But without understanding organizational strengths and weaknesses related to adopting change and improving outcomes, many organizations struggle to successfully implement initiatives to reduce unnecessary clinical variation.
UnityPoint Health is the nation’s 13th largest nonprofit health system and the fourth largest nondenominational health system in America. As a network of hospitals, clinics, and home care services, UnityPoint Health provides care throughout Iowa, western Illinois, and southern Wisconsin. UnityPoint Health leaders knew that an understanding of organizational strengths and weaknesses related to adopting change and improving outcomes would be critical to enhance its ability to successfully execute outcomes improvement and consistently realize the intended benefits of its improvement efforts.
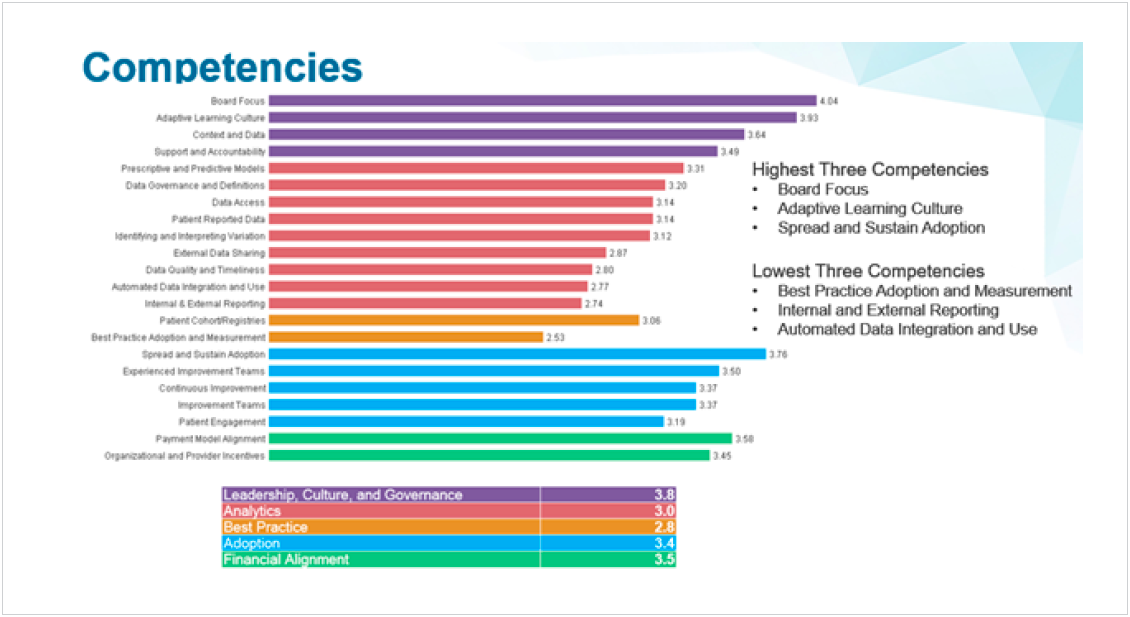
UnityPoint Health selected the Outcomes Improvement Readiness Assessment (OIRA) Tool and professional services from Health Catalyst to conduct the assessment and interviews to obtain an informed and data-driven assessment of its organizational competencies. The results of this assessment identified the strengths and weaknesses of UnityPoint Health related to executing outcomes improvement, and defined the competency level at the organization, facility, and department levels along five parameters:
After the assessment was complete, UnityPoint Health discovered that it trailed behind benchmarks for organizational competency in analytics, best practice, and adoption. Specifically, the information indicated a need to improve best practice adoption and measurement, internal and external reporting, and automated data integration and use.
The strengths that UnityPoint Health could draw upon were also identified in the assessment and showed that compared to benchmarks, UnityPoint Health had a strong board focus, an adaptive learning culture, and the ability to spread and sustain adoption. At the same time, it performed the readiness assessment, UnityPoint Health leveraged the Key Process Analysis (KPA) application to identify potential improvement opportunities and determine which of those efforts would provide the most benefit to patients and the organization. Leadership then set out to determine how to best use the recommendations, data, and insight obtained from the OIRA Tool and the opportunity analysis to develop an effective approach to outcomes improvement that would consistently deliver and sustain the intended benefits to patients and the organization.
UnityPoint Health began by focusing on its strengths and further bolstering its leadership, culture, and governance by tackling the readiness assessment recommendation to improve the process for prioritizing projects, recognizing that without a tightly held rallying point, organizational motivation and focus would be diluted, resources would be wasted, and objectives would not be achieved. The prioritization process needed to deliver a short list of impactful improvement projects that would provide high value and could be completed with the available resources.
With the list of potential improvement projects in hand, UnityPoint Health determined that for the prioritization process to be fully informed, it needed additional input from subject matter experts that could take into consideration the competency levels and capacity of the departments that would be impacted, validate the projected savings from the opportunity analysis, and assess the availability of strong clinical champions. UnityPoint Health engaged the subject matter experts for each clinical domain to fill in these more subjective analyses and further define the interrelationships of the projects under consideration.
The organizational competency assessment indicated organizational deficits in analytics, adoption, and best practice (see Figure 1). Delving deeper into the information, UnityPoint Health was able to gain greater insight into these findings and design a plan to increase competency in those three areas to support the teams who would be working on improving outcomes.
The competency assessment identified the need for UnityPoint Health to increase its analytics capabilities, but UnityPoint Health knew that analytics without confidence in the data is practically useless. The ability of any given organization to successfully and sustainably address inappropriate variation in care delivery is highly dependent on access to credible data.2 To successfully obtain the support of stakeholders for data-driven prioritization and outcomes and performance monitoring, UnityPoint Health needed to provide leaders with a credible, single source of truth that was accepted by all leaders. Leveraging the Health Catalyst® Analytics Platform and broad suite of analytics applications, UnityPoint Health was able to meet this demand by providing expanded drill down data access and regional-level data in its analytics applications which made the data useful and validated its accuracy in the eyes of its stakeholders.
Having obtained the confidence of its leaders and stakeholders, UnityPoint Health further increased its analytics capabilities by developing data sources, visualizations, and analyses to monitor and assess priorities, progress, and outcomes. This led to expanded use by improvement teams and operational leaders that made it possible for UnityPoint Health to uncover pockets of excellence that could be spread, as well as identify areas of poor performance and intervene appropriately to change clinical practice.
To further support this expansion of analytics capabilities and adoption, UnityPoint Health committed to the continued development of analytic skills and training across the regions to ensure that analysts had the ability to keep up with the increased demand for information generated by a data-driven organization. Recognizing the need to prioritize resource allocation, UnityPoint Health decided that whenever necessary it would narrow the analytics development to the clinical domains that had been selected as prioritized improvement projects, supporting data needs that would lead to improved outcomes.
It is possible to have excellent analytics applications and credible data, and still not improve outcomes if the tools and information are not widely used and integrated into practice. UnityPoint Health recognized that the first step to ensuring widespread adoption was to communicate all decisions, progress, and accomplishments across the entire organization, thus gaining awareness, understanding, and support for the prioritized projects. Next, UnityPoint Health expanded the user base and gained greater adoption of the analytics applications.
Communicating the strategy and gaining adoption across three states and multiple organizations can be challenging. Playing to the “what’s in it for me?” side of human nature, UnityPoint Health leveraged the drill down capability built into its analytics applications to provide views that would provide valuable information to everyone —increased adoption soon followed.
UnityPoint Health also determined that support for the prioritized projects would be stronger if the work of the improvement teams were aligned with both clinical and operational initiatives so that all parts of the organization could recognize the benefits from improved outcomes. The resulting demand for multiple, integrated layers of information across the organization was met by the analytics applications providing greater reporting capability that included meaningful regional and site comparisons.
Recognizing the need to focus on clinical improvement to achieve best practice and reduce clinical variation, clinicians across the organization continued their work of reviewing and cleaning up order sets and aligning the workflow and EMR optimization. During this phase, it was important to monitor the engagement of clinical workgroup teams to avoid work overload, so a mid-tier engagement group was developed to assist in the deployment of best practice across regions.
With a prioritization strategy in hand, and credible analytics to provide vital and easily accessible information to support data-driven decisions, leaders engaged clinical practice domain and workflow experts to expand upon the details and interrelationship of the projects under consideration. This work provided a complete picture of each proposal and of the effort needed to deliver the expected benefit. The ultimate goal was to create and present a short list of projects to leadership with the confidence that they could be successfully and concurrently implemented to improve patient outcomes.
Knowing that the organizational priority was to reduce unnecessary variation—and using the opportunity analysis as a starting point— stakeholders started by asking themselves where they could reduce variation and improve outcomes most quickly and effectively. The underlying assumption was that projects should be selected based on the magnitude of benefit as well as ease of execution. It was assumed that reducing clinical variation could be more easily accomplished where best practice was well-defined.
The stakeholders identified clinical areas where guidelines, protocols, and order sets had already been developed and implemented to guide and improve best practice. Those clinical domains had prior experience, were further along in the process, and therefore more likely to adopt and standardize to best practice. Another critical piece of the puzzle required analyzing what areas of the organization would be impacted by each project. For instance, working on sepsis would impact the ED, so if the sepsis project was selected, other projects that also utilized ED resources would need to be eliminated or delayed. In addition, UnityPoint Health had to weigh the availability of a project champion. Clinical projects would require a strong clinical advocate and leader that could build collaboration and drive adoption of changes to clinical practice. If no champion was available, the project was removed from consideration.
Now, with priorities set, and a plan in place to improve competency levels for analytics, adoption, and best practice, UnityPoint Health embarked upon the journey to improve clinical practice for septicemia, CAD/AMI, diabetes, and COPD.
An improvement team was created for each prioritized clinical domain. Team members included clinical subject matter experts and a change management expert. In some cases, it was possible to find one individual that had both skill sets and was able to fulfill both roles for their team. Each team also had an analyst and a process engineer assigned to build or revise the analytics application, complete the analysis, and present results and process measures to operational leaders. Analyst and clinical communications were improved by working closely together to design and improve the measurement and reporting of best practice.
To save time in the long run, and set the stage for successful execution, the teams were given the time to consider the multilayered facets of the project before beginning the work. Because the OIRA Tool framework provided visibility at a department level into what strengths they could depend on and what weaknesses might create barriers, the improvement teams spent extra time upfront to plan properly. This slower approach, in the beginning, enabled the improvement team to avoid barriers wherever they could and create a plan to overcome any barriers when that was not possible.
Improvement team leaders each committed to using the information and framework of the readiness and competency assessment which resulted in everyone referencing the same playbook and speaking the same language. This shared framework made it possible for the teams to see the benefit of having leadership, analytics, and best practice work together to make progress in a coordinated fashion in all three areas, with leadership driving best practice in partnership with analytics, and the entire organization learning how those pieces fit together. This approach led to improved outcomes in each of the prioritized clinical domains.
The UnityPoint Health leadership team is committed to using data-driven insights to drive outcomes improvements. In the first six months following the deployment of best practice interventions to improve care for patients with sepsis, a number of improvements were achieved:
Additional results are being recognized in other domains, including a 10 percent increase in the percent of cardiac stent placements that are occurring via the radial approach.
“We wanted to reduce variation that did not provide value to patients and saw the readiness assessment as an objective methodology to determine the path forward that would be the most successful.”
– Rhiannon Harms Executive Director, Analytics
UnityPoint Health plans to continue to review the KPA application to identify large improvement opportunities throughout the year aligned with its strategic planning cycle and the priorities identified by clinical and operational leadership.




