Heart failure (HF) is the leading cause of hospitalizations among adults over 65 in the U.S, costing Medicare over $17 billion annually. To address this challenge, Allina Health implemented a multidisciplinary HF management program with nurse care coordinators and nurse practitioners to enhance patient engagement and ensure coordinated care. Utilizing data from its enterprise data warehouse, Allina has successfully reduced 30-day HF readmission rates.
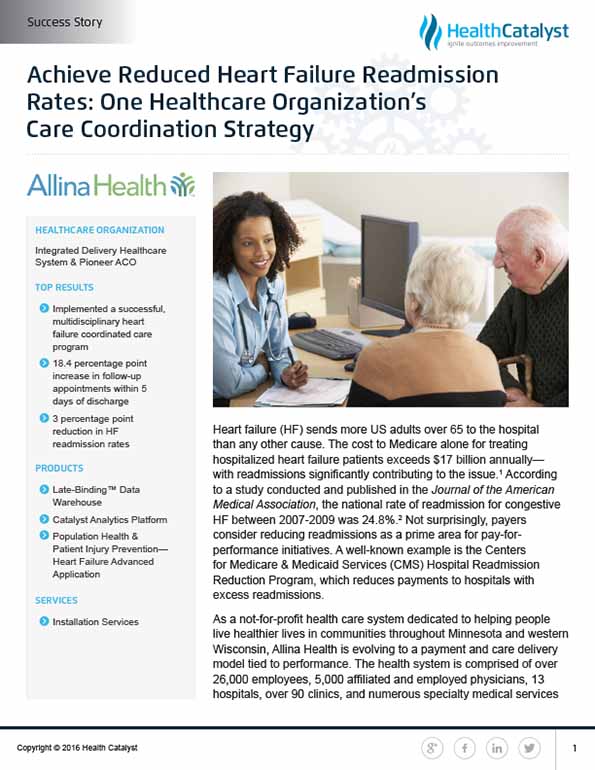
Heart failure (HF) sends more US adults over 65 to the hospital than any other cause. The cost to Medicare alone for treating hospitalized heart failure patients exceeds $17 billion annually— with readmissions significantly contributing to the issue.1 According to a study conducted and published in the Journal of the American Medical Association, the national rate of readmission for congestive HF between 2007-2009 was 24.8 percent.2 Not surprisingly, payers consider reducing readmissions as a prime area for pay-for- performance initiatives. A well-known example is the Centers for Medicare & Medicaid Services (CMS) Hospital Readmission Reduction Program, which reduces payments to hospitals with excess readmissions.
As a not-for-profit health care system dedicated to helping people live healthier lives in communities throughout Minnesota and western Wisconsin, Allina Health is evolving to a payment and care delivery model tied to performance. The health system is comprised of over 26,000 employees, 5,000 affiliated and employed physicians, 13 hospitals, over 90 clinics, and numerous specialty medical services that include pharmacies, hospice care, home care and emergency medical services. While Allina has a long history of providing high quality care, they also recognized that they were not well organized to provide care in an emerging environment of population health management and outcome-based reimbursement.
When CMS originally announced its focus on heart failure admissions, Allina’s own 30-day readmission rates were generally running well above 20 percent. This higher-than-desired rate could be improved, Allina believed, with more coordinated care.
However, like most other healthcare systems that have historically been structured to operate in a fee-for-service world, Allina was not well organized for coordinated care delivery. Patients with chronic conditions like HF touch so many different providers at different times and locations that it is difficult to know exactly who “owns” the patient’s overall care management across the continuum of care.
In the inpatient environment, for example, the nurses and physicians (hospitalists and cardiologists) attending to the patient typically do an excellent job. However, their focus is exclusively within the four walls of the hospital setting. Post-discharge, patients are largely on their own until readmission or until they are seen in the clinic. Similarly, when patients are seen in the clinic, outpatient providers do an equally good job, but once the patient leaves the clinic, they are once again largely on their own until readmission to the hospital or until another clinic visit. Care providers tend to operate in “silos” with no one entity or provider managing the process across the continuum of care. Just as care is in silos, data often is in silos as well—data that, if integrated and easily accessible, could reap important insights for providing more coordinated care and reducing readmissions.
Allina recognized that all providers in HF management were working hard and deeply committed to their patients’ full recovery. However, someone had to take ownership of the overall care management process for HF. The health system also recognized these providers could have a profound impact if they could work together in a more coordinated, collaborative, and data-driven fashion.
Shortly after CMS announced its focus on HF readmissions, Allina’s Mercy Hospital launched a multi-year effort to improve the care of HF and reduce 30-day HF readmissions. Cardiologists stepped forward and agreed to assume responsibility for improving the care of HF patients. Using dedicated resources within the cardiology group, processes were put into place to improve care coordination and provider collaboration. This ultimately achieved a significant reduction in readmissions from 24 percent to 14 percent. Taking note of Mercy’s success, Allina eventually decided to roll out a full-fledged HF management program, supported by a late-binding data warehouse from Health Catalyst that pulls in essential data across the enterprise. This platform in turn supplies information to HF analytics dashboards that enable Allina care providers to monitor, analyze, and manage a diverse set of HF care and performance metrics.
The HF management program is designed to overcome persistent challenges with care coordination—particularly lack of a clear ownership of the HF care management process. The program focuses on five major functional areas: nursing, care coordination, protocols and guidelines, measurement and reporting, and education. Each functional area is led by a cardiologist, with care coordination co-led by a cardiologist and a primary care physician. Care is then supported by a multidisciplinary team that includes specialists, nurses, therapists, hospitalists, rehab, palliative care, and others. Evidence-based guidelines are drawn from national societies, such as the American College of Cardiology.
The overriding goals of the program are to assure a consistent approach among all clinics and hospitals; integrate appropriate services such as palliative and rehab care with the care process; and of course, coordinate care across the continuum. To help drive these objectives to fruition, Allina has put an executive committee in place that consists of leaders of the functional area teams and the overall physician lead. They follow a highly collaborative, relationship- centered approach to build engagement and an environment of trust. A key strategy is to encourage all involved in HF care to look beyond their individual roles to identify gaps in care and determine how to improve overall care coordination.
A nurse HF care coordinator role was also created. This individual goes into the hospital to see HF patients, understand their care plans and assure that the plan is executed after discharge. The coordinator is “silo-less” and serves as the “bridge” to help manage care for the patient across the continuum, regardless of the care setting or environment. In addition, nurse practitioners help fill the need for timely follow-up appointments after discharge, to manage medications and help assure the patient is stabilized.
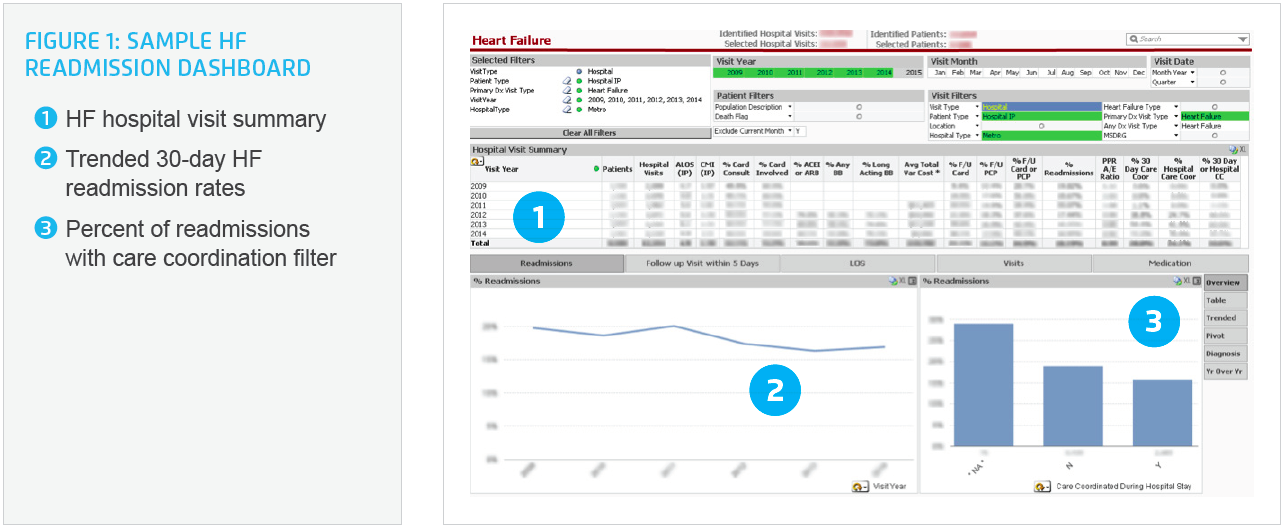
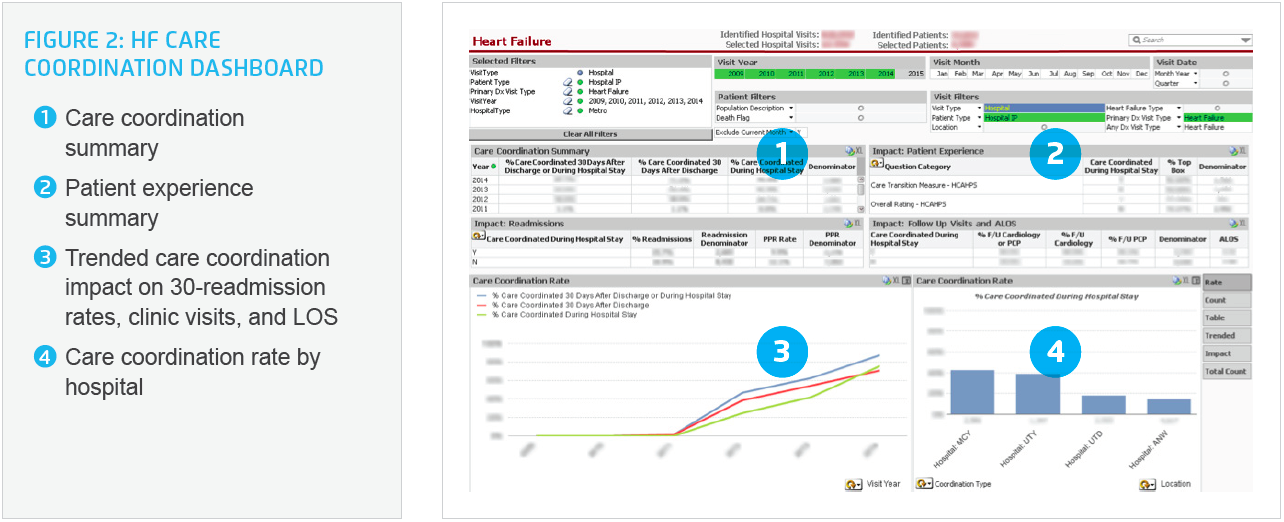
The enterprise data warehouse aggregates clinical, financial, operational, patient experience, and other data to create consistent views of the data that inform decisions. The advanced HF analytics dashboard monitors and manages performance (see Figure 1). It is also used to drive behavior change and as a “case finding tool”—such as identifying high-risk patients that may need more focused treatment or palliative care. The impact of care coordination is monitored (see Figure 2), as well as end of life management (see Figure 3).
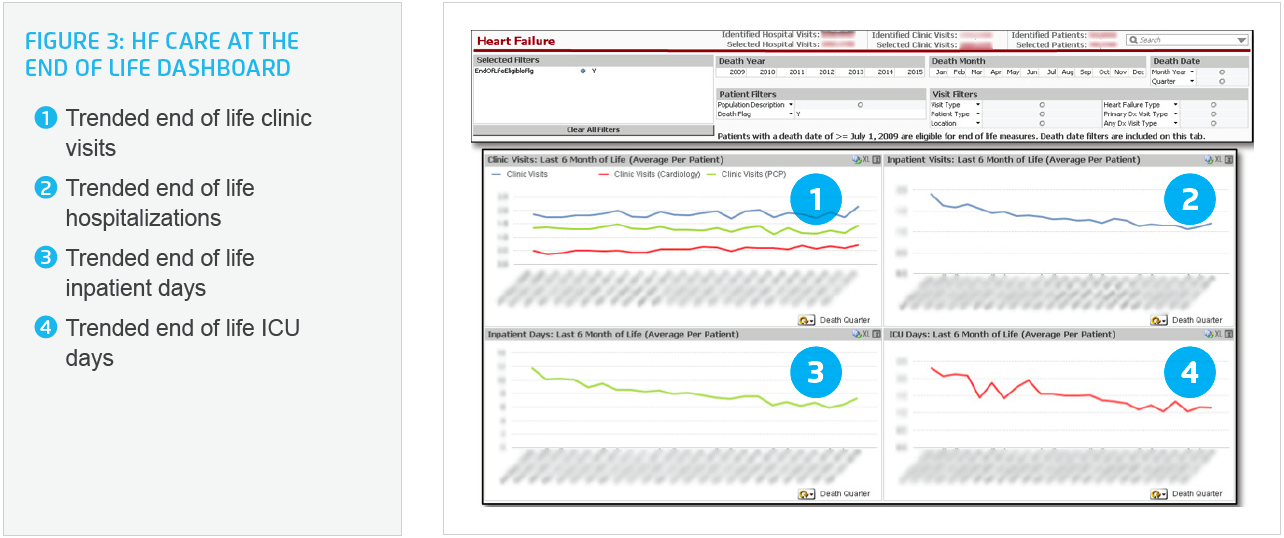
The leadership of the HF program recognized that there are two key outcomes that really matter—length of life (mortality) and quality of life (QOL). While length of life can be measured relatively easily, assessing QOL requires more effort. It is important information, however, that helps provide safe, appropriate and effective care to the patient.
Allina uses the Patient Reported Outcomes Measurement Information System (PROMIS) survey to measure health status. Funded by the National Institutes of Health,3 PROMIS is a system of precise measurements of patient-reported health status of physical, mental, and social wellbeing. PROMIS surveys, for example, measure what patients are able to do and how they feel. Based on experience, Allina has found that patients want their care providers to understand and use this information in their care.
Allina has made notable progress with its HF management program. Cardiologists and PCPs have played important leadership roles while the use of nurse HF coordinators and nurse practitioners has been central to the program’s success. All have been considerably aided by an effective clinical decision support and analytic infrastructure to monitor outcomes, manage the heart failure population, and help drive culture change.
Meaningful reduction in HF readmission rates. Through the implementation of a HF Care Coordination program, Allina achieved an overall three percentage point reduction in HF readmission rates in the metro hospitals, from 19.7 percent to 16.7 percent. By using a relationship-centered, highly collaborative and data driven approach, care provider acceptance of and engagement in the HF program has been greatly facilitated resulting in a significant reduction in 30-day readmissions.

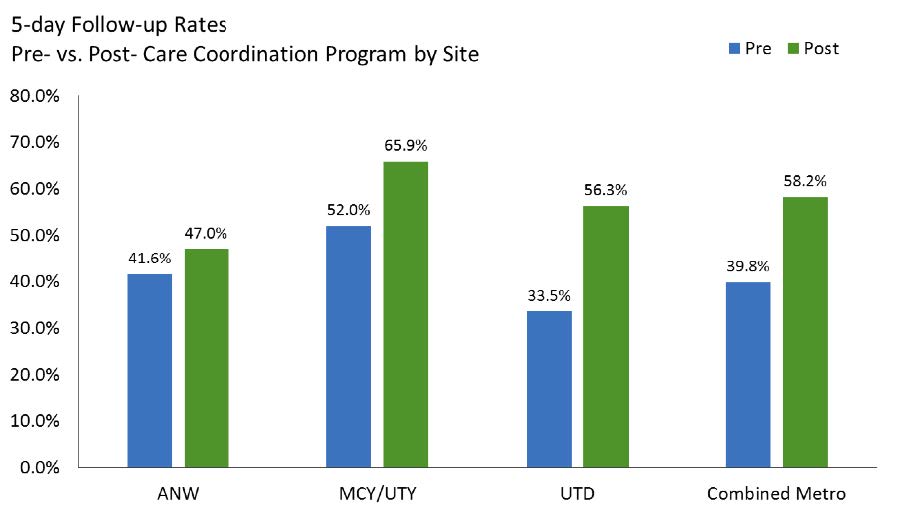
Significant increase in appropriate post hospital follow-up care. There has been meaningful improvement in successfully identifying HF patients who would benefit from care coordination efforts, which has resulted in an 18.4 percentage point increase in post hospital follow-up clinic appointments within five days, from 39.8 percent at baseline to 58.2 percent post implementation.
"Analytics is the jet fuel of the heart failure program. Without a doubt, access to good data drives cultural change. This has elevated heart failure management at Allina to an outstanding program.”
– Spencer Kubo, MD, HF Program Medical Director, CV Clinical Service Line
With the results of coordinated care made clear, Allina will continue to build upon this strategy and expand uses of the technology that supports it. In the near future, for instance, Allina plans to capture data regarding compliance with best practice protocols and HF care plans. In addition to 30-day readmissions, focus will soon broaden to include readmissions at six and 12 months. Allina also plans to improve the rate at which newly diagnosed patients are entered into the HF program, and the quality and length of life rates for these patients.
Yet another objective is to measure the financial impact of the HF program. With such significant drops already in readmissions and ED visits, the clinical impacts are already plainly apparent.