At MultiCare Health System (MultiCare), inconsistent application of improvement methods, differing competencies, misaligned projects, and inefficient performance data collection were impeding the organization’s ability to improve, leaving quality and operational metrics below expectations. Using a data platform and a robust suite of analytics applications, MultiCare has integrated analytics support into its improvement teams, reducing hospital length of stay (LOS), and achieving significant cost savings.
U.S. hospitals see more than 35.7 million stays each year, costing more than $417 billion. The average LOS is 4.6 days, with the average cost per day at $11,700.1 Even a minor reduction in LOS can produce substantial cost savings. Reducing LOS also benefits patients, as long hospital stays increase the risk for hospital-acquired conditions, such as a pressure injury or infection.
In pursuit of continuous process improvement, MultiCare sought to build a best-in-class culture in which nurse leaders use the best data and methods to continually drive improvement at a unit level. Despite this desire, the organization had not yet achieved its goals.
Inconsistent application of improvement methods, differing levels of competency, misaligned projects, and the time-consuming performance data collection were impeding the organization’s ability to improve. Quality performance and operational metrics, such as LOS, were not meeting the organization’s expectations. MultiCare needed a plan that would enable its nurse leaders to consistently use improvement science and data to drive continuous improvement.
MultiCare partnered with Health Catalyst to build a best-in-class culture, with nurse leaders effectively driving unit-level improvements. The organization established a governance system for improvement work, ensuring that improvement activities are aligned with the larger organizational goals. MultiCare and Health Catalyst clinical and process improvement subject matter experts developed and implemented a standard improvement methodology.
MultiCare provided development opportunities to increase its nurse leaders’ competency and effectiveness in leading continuous process improvement. With training and 1:1 at-the-elbow support for improvement work, Health Catalyst clinical and process improvement experts embedded at various MultiCare facilities coached the nurse leaders in learning and applying the correct methods to understand complex challenges and drive evidence-based improvement.
Nurse leaders at MultiCare applied their learning to LOS challenges, using a data-driven approach to enable the organization’s standard improvement methodology to improve patient flow and progression of care. The organization implemented standard work, including the following:
MultiCare uses the Health Catalyst® Data Operating System (DOS™) platform and a robust suite of analytics applications for its data and analytics needs. The organization integrates analytics support into its improvement teams, ensuring that analytics drive outcomes.
The organization uses the Leading Wisely analytics application to efficiently monitor the effectiveness of its improvement efforts (see Figure 1). The analytics application does not require extensive technical skills, empowering leaders at all levels to visualize, monitor, share, and report information.
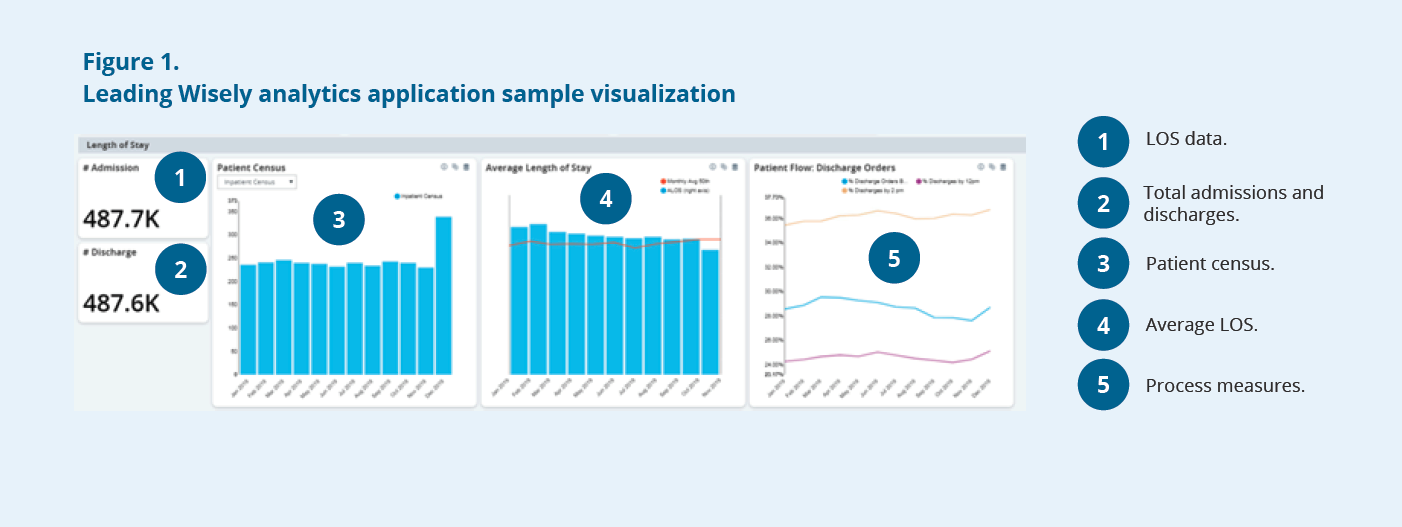
Nurse leaders can use the analytics application to monitor quality and operational data, including data for catheter-associated urinary tract infections, central line-associated bloodstream infections, hospital-acquired pressure injuries, hospital-acquired Clostridioides difficile infections, fall events, LOS, and patient satisfaction.
MultiCare’s efforts to create a data-driven, continuously improving organization are delivering the desired results, including a:
“By using a data-driven improvement methodology, we’ve empowered our teams, who were able to successfully reduce length of stay, saving $24M annually. Our teams now have the skills, and the data and analytics, to help them sustain the gains.”
– June Altaras, MN, NEA-BC, Senior Vice President & Chief Quality, Safety & Nursing Officer
MultiCare plans to spread and scale its data-driven improvement methodology across the entire organization.