El Camino Hospital aimed to reduce hospital length of stay (LOS) while ensuring patient safety. Facing challenges in improving discharge processes and identifying key issues, the hospital implemented analytics and multi-disciplinary cooperation to identify high-risk patients and enhance discharge care coordination, ultimately focusing on quality and cost reduction.
U.S. hospital stays cost the health system at least $377.5 billion per year. In today’s value-based care environment, hospitals are under increasing pressure to avoid patient harm and maintain quality while also lowering costs. Reducing hospital length of stay (LOS), especially as it relates to avoiding unnecessary hospital-acquired conditions (HACs), is a primary indicator of a hospital’s success in achieving these goals.
El Camino Hospital, a 395-bed multi-specialty community hospital in Mountain View, Calif., places a high priority on keeping patients safe. However, when it came to its goal of reducing LOS, leaders recognized that they faced some major challenges, including:
By implementing analytics and protocols that provide access to actionable data, the LOS reduction team was able to identify patients at high risk for increased LOS so that they could develop and track critical interventions. El Camino Hospital’s patient-centered approach to tackling LOS reduction also included multi-disciplinary cooperation, leadership buy-in, and additional resources to enhance discharge care coordination.
El Camino Hospital, a 395-bed multi-specialty community hospital in Mountain View, Calif., places a high priority on keeping patients safe. Leaders of the hospital—which has been recognized with magnet status for nursing excellence by the American Nursing Credentialing Center—recognize the important role that length of stay (LOS) plays in patient safety.
Driven by mounting pressure from both public and private sectors to avoid patient harm and lower costs, reducing LOS had become a top priority not just for El Camino Hospital, but for hospitals and health systems across the nation.1 With hospital care costs in the United States reaching $377.5 billion per year,2 addressing length of a hospital stay can positively impact that number. A longer LOS also increases the likelihood of a hospital-acquired condition (HAC), which harms patients and contributes to an even longer and costlier stay.3
In addition to improving patient safety and lowering costs, reducing LOS can release capacity in the system (including beds and staff time) and improve throughput, enabling the hospital to serve more patients. And although shorter LOS has been correlated with a significantly higher risk of readmission in multiple studies and countries,4 the results of El Camino Hospital’s improvement efforts demonstrate that these risks can be mitigated as hospitals seek the optimal LOS for maximizing quality and minimizing cost.
While many healthcare organizations are interested in reducing LOS, effecting change can be challenging due to the complex and multi-layered nature of the problem and the many disciplines that need to be involved in the solution. El Camino Hospital leaders knew that in order to be successful, they would need to leverage real-time, targeted analytics to identify obstacles and measure improvements.
In addition, a multidisciplinary approach would be essential to improve the entire discharge process.
El Camino Hospital recognized that reducing LOS would be a major undertaking due to the complexity and scope of the related issues. The team working on this initiative identified the following challenges and potential barriers and laid out the groundwork to overcome them:
The team knew that implementing and sustaining LOS improvement efforts would require ongoing communication, collaboration, and alignment between the hospital and the community, between providers, and with patients and families. As such, everyone in the organization—from the executive team to clinicians on the frontlines of care—would need to embrace and own the initiative. To make this happen, El Camino Hospital needed key leaders within the hospital to recognize and support the importance of reducing LOS.
Measuring and tracking LOS can be a difficult and complex matter, and El Camino Hospital’s historic method of doing so was imprecise. Without timely and actionable data or insights, El Camino Hospital was hampered in its improvement efforts. Team members recognized that their efforts might fail if they weren’t able to pinpoint the clinical, operational, and financial factors driving LOS. They needed a way to identify the interventions to focus on that would have the most impact. They also had to ensure that related measures (such as readmissions) would not be negatively affected by their LOS interventions.
Managing variation in the discharge process and systematically identifying and addressing clinical and operational barriers to a timely discharge were pivotal priorities for El Camino Hospital in its efforts to decrease LOS. El Camino Hospital’s team recognized that it had a variable and unpredictable discharge process.
Many factors contributed to the variability in discharge practices. Chief among these was a lack of resources, which hampered discharge planning. Many care coordinators managed too large a patient panel and could not spend enough time with individual patients. Care coordinator coverage did not adequately include all shifts and weekends or the emergency department (ED).
Furthermore, some discharges presented problematic barriers that were difficult for staff to address. Such barriers included:
The hospital needed more timely and consistent communication about discharge barriers with providers, families, and the community.
El Camino Hospital’s overarching goal was to reduce LOS while keeping readmissions stable. Its principle motivation for reducing LOS was to improve quality and outcomes for patients. Involving them in care decisions and transitions was a key component of the initiative. Ensuring that patients were the focus of these efforts led El Camino Hospital to make different and better decisions than if it had focused primarily on financial or operational outcomes.
The success of El Camino Hospital’s efforts hinged on three components, including leadership and organizational alignment, accurate and accessible data and analytics, and patient-centered operational efforts.
Reducing LOS required changes in processes and practices; therefore, it was critically important to obtain executive, clinical, and operational engagement prior to launching the project. Maintaining alignment across the C-suite had to be an ongoing and multidisciplinary effort across business, operations, and clinical leaders.
El Camino Hospital’s chief medical officer (CMO) and chief nursing officer (CNO) were active champions of the LOS project, which was tied to the many of the organization’s strategic goals and objectives. The chief operation officer (COO) added the project to the agenda for the Operations Council, and leaders spoke about their efforts to support the initiative. This kind of high-profile, high-visibility support led to widespread ownership and engagement. In addition, a tactical group, the LOS steering committee, prioritized work, monitored variances, and tracked progress.
Measuring and managing ALOS is complex because it has multiple dependencies and impacts other metrics. Understanding the underlying dynamics, identifying and targeting key opportunities,and observing blockages in patient flow requires tracking and understanding of multiple metrics—and they all hinge on access to consistent, accurate data and the ability to drill down into that data.
To gain these capabilities, El Camino Hospital implemented an enterprise data warehouse (EDW) and analytics platform enabling the team to integrate data from numerous source systems, including clinical, billing, cost, and quality.
The analytics applications facilitate the presentation of LOS information in an effective, easy-to-use, and actionable manner (Figure 1). The team specifically found that it was important to get the data to the unit managers so they could use the information in their shift huddles and educate nurses on what their role is in reducing LOS. This approach to data transparency broke everyone out of their silos and led to better communication.
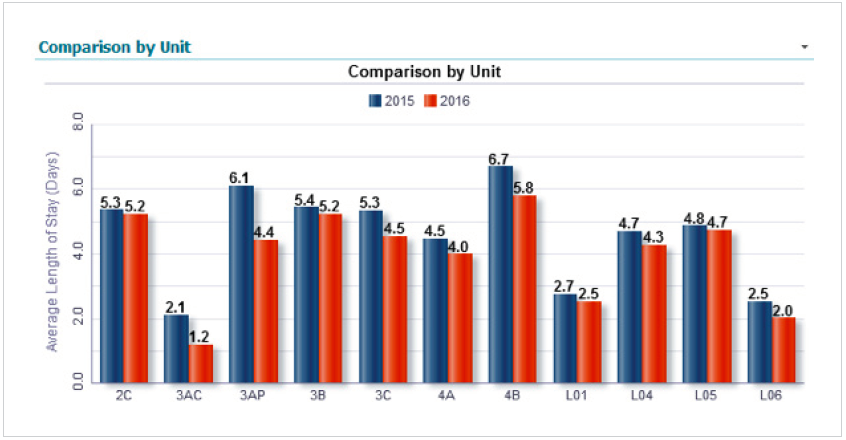
Having timely and actionable data in an easy-to-digest format proved key to the project’s success in many other ways. For example, the data allowed for better identification of issues contributing to a long LOS, especially in areas where team members did not realize there was an issue. At the outset, the project focused on all patients and all payers, but as the team delved into the work, the data revealed that two major outliers were contributing to the increased LOS for El Camino Hospital—oncology patients and Medicare patients in the acute and intensive care units (ICUs). Armed with this information, the team began targeting interventions and processes to impact the patients with the biggest opportunities for improvement, while tracking which interventions made the most difference.
El Camino Hospital initially used ALOS as a measure but found it to be too high-level, generic, and delayed to be useful. Team members needed a different metric and wanted the data to show it in a consumable way. Their solution was to create a new, customized way to conceptualize LOS, which they called “days stayed.” This measure looks at total days consumed or used, then focuses on the high-utilization patients responsible for long stays (Figure 2).

This new way of understanding and visualizing data via “Days stayed” enabled El Camino Hospital to track patients who were deemed dischargeable but who were still in the hospital. They then moved these patients into a virtual SNF (VSNF), which allowed them to track two LOS measurements: one with all patients and another with the VSNF patients excluded. This separation enabled the team to focus LOS improvement efforts to specific patient sets. For example, the data revealed that patients staying longer than 19 days accounted for 42 percent of the total “Days stayed.” Focusing on those more complex patients and their specific barriers to discharge allowed the team to make a significant imp act on overall LOS.
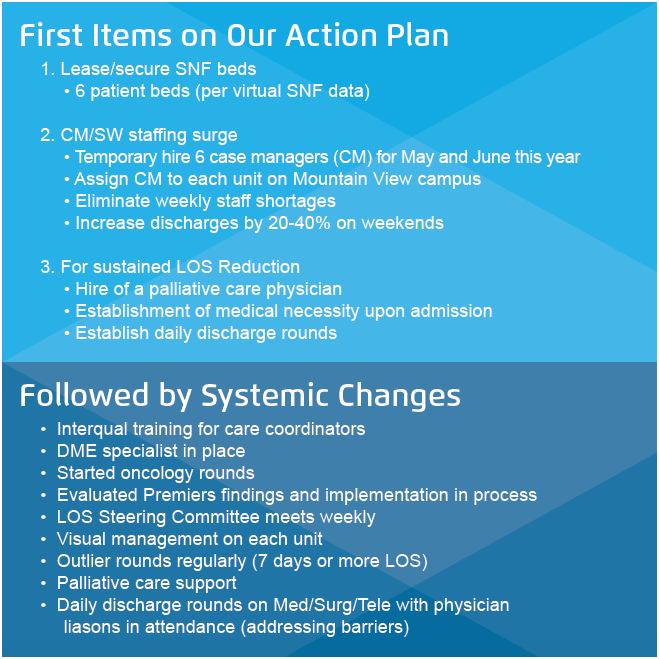
El Camino Hospital created and followed a thoughtful and thorough action plan as it strove to implement a patient-centered initiative for optimizing LOS. The key actions and systemic process changes that contributed to the success of the LOS reduction program (summarized in Figure 3) included:
Not only did El Camino Hospital exceed its ALOS reduction target, but it also achieved reductions in readmissions and demonstrated that reducing unnecessary days in the hospital is directly correlated with reducing HACs and patient safety indicators (PSIs). These improvements in quality and outcomes also resulted in significant cost savings. In addition, El Camino Hospital has improved bed capacity and throughput as a result of the initiative and is better managing expenses such as supplies and staffing.
Improvements in key metrics have included:
El Camino Hospital is proud of the teamwork and collaboration that drove these improved patient, financial, and operational outcomes. Leaders emphasize the importance of focusing on a patient-centered approach for a better patient experience. They attribute the initiative’s success to aligned goals, to access to actionable data—and particularly to the dedicated work of a cross-functional, multidisciplinary team that engaged the staff, the patients, families, and the community in its work.
“It was critical for us to help attending physicians know that we were trying to help them and their patients—not to take control of the patient’s care.”
-Michelle Pezzani, MD, Medical Director, Utilization Management, ECH
The groundwork of the initial LOS reduction program has set the stage for future enhancements, including:
The LOS reduction team will remain in place so that the initiative remains a leadership priority. The team continuously monitors processes and measures to sustain the progress they have made. Meanwhile, their focus on expanding access to timely and reliable data continues.