Mixed reviews on pay-for-performance programs challenge hospitals in enhancing patient care. MultiCare’s initiatives in pneumonia, sepsis, and women’s health showed improvement, but the organization sought further enhancements. MultiCare formed a shared-risk partnership with Health Catalyst, establishing a framework and governance structure via a Shared Governance Committee to prioritize and align improvement initiatives.
Mixed reviews of the effectiveness of pay-for-performance programs leave hospitals wondering how to affect meaningful change in patient care and outcomes. However, MultiCare’s experience with focused improvement efforts supported by analytics for pneumonia, sepsis, and women’s health showed that better data consistently leads to better patient outcomes.
Committed to improving population health, and informed by their experience as well as national trends and outcomes, MultiCare formed a new partnership with Health Catalyst, a next-generation data, analytics, and decision support company. The shared risk partnership generated an improvement framework and governance structure formed around a Shared Governance Committee which is responsible for prioritizing, resourcing, and aligning improvement initiatives across MultiCare. The committee and the projects it ultimately approves are informed by data-driven opportunity analysis and ongoing analytics support.
The U.S. healthcare industry is in the midst of a shift in focus from individual to population health. Numerous metrics are in place to measure the impact on quality, outcomes and patient experience, with commercial payers and CMS increasingly paying for outcomes achieved instead of services rendered.1 Evidence of the effectiveness of these value-based reimbursement programs is mixed.
The Hospital Value-Based Purchasing program, for example, has not been able to deliver on the goal of lowering mortality rates. As a result, in 2016 researchers concluded that nations considering similar pay-for-performance programs may want to consider alternative models to achieve improved patient outcomes.2 At the opposite end of the spectrum, similarly structured penalty programs in the U.S. have seen a 21 percent reduction in hospital-acquired conditions between 2010 and 2015.3
With such contrasting results, hospitals are understandably wondering: what makes one program work and the other one fail? Ultimately, what is the secret to driving outcomes improvement?
MultiCare, an integrated healthcare delivery system in the Pacific Northwest, had experience with focused improvement efforts supported by analytics for patients with pneumonia, sepsis, and hysterectomies which showed that better data consistently leads to better patient outcomes. Executive leadership determined that to deliver on their mission to create a healing and healthy future, MultiCare needed a data-driven way to consistently produce sustainable and meaningful improvements that would not only contribute to the health of individual patients, but to the population as a whole. This strategy would promote MultiCare’s vision of being the Pacific Northwest’s highest value system of health by including not just quality outcomes, but also improvements in service excellence and affordable care.
MultiCare was faced with three major obstacles in implementing its strategy.
To overcome these obstacles, MultiCare determined that the best approach was to leverage their existing business relationship with Health Catalyst. Health Catalyst had provided the analytics platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications that supported the analytics for MultiCare’s previously mentioned success with clinical improvement projects. It was a natural evolution of their business relationship to join forces to operationalize a framework that would consistently produce sustainable and meaningful improvements in clinical outcomes, patient experience, and cost.
The vision of the partnership between MultiCare and Health Catalyst was twofold: first, to raise the awareness of using data analytics to drive improvement in healthcare; and second, to build a strong base of users that can use analytics tools to help take care of patients, recognize patterns, and use early identification to identify and manage populations.
To meet these objectives, MultiCare and Health Catalyst set out to structure the partnership around certain core components that would overcome the previously identified obstacles. These include:
The partnership was grounded in a shared risk model, whereby MultiCare and Health Catalyst have agreed to go at risk financially in terms of payment that will be based on their shared success.
Having committed to the partnership, the next step was to establish a strong framework for implementing the use of analytics for outcomes improvements. The framework is based on four key governance principles: engage stakeholders around a common vision; establish a shared understanding of organizational needs, capabilities, and readiness; create alignment with a consistent improvement methodology, incentives, and priorities; and, keep focused on practicing disciplined decision making to prioritize, fund, organize, and sustain initiatives that require analytics.
Engaging stakeholders across the organization. MultiCare’s executive vice president and chief operating officer started the new partnership by sending out a call to action to rally the organization around MultiCare’s mission and vision, informing the leaders about the intent and goals of the new partnership with Health Catalyst. A leadership team was formed, the Shared Governance Committee, which was given the highest level of accountability for analytics resources and funding across the MultiCare integrated healthcare system. Members of the Shared Governance Committee were carefully chosen to provide the right mix of knowledge, skill, and influence.
The committee is comprised of senior executives from MultiCare representing operations, finance, quality, and medicine, and three representatives from the Health Catalyst executive leadership team. The inclusion of a financial expert was considered essential to ensure that outcomes were quantified and cost savings accurately represented. The partnership felt it was important to improve clinical outcomes, and service and operational excellence through changes that were not only effective, but scalable as well, and ultimately made care more affordable. They were committed to ensuring an overall cost model that generates revenue that can be reinvested in the community. Inclusion of clinicians’ voices from the Clinically Integrated Network and the existing quality improvement Clinical Collaboratives program was considered equally important to ensure
continuation of their successful improvement programs and seamless integration of quality initiatives across the enterprise. By ensuring that all of the appropriate voices are at the table when decisions are made, and that all decisions are transparently communicated across the organization, all stakeholders become part of the process.
Establishing a shared understanding. To create a high level of shared understanding among the members of the Shared Governance Committee, MultiCare stakeholders participated in an in-depth readiness assessment focused on identifying MultiCare’s specific needs, capabilities, and readiness to become a Center of Analytics Excellence and a data-driven organization.
The Shared Governance Committee also leveraged information from its Key Process Analytics application to conduct an opportunity analysis. This robust application enabled different views of patient populations, helping to uncover opportunities for reducing clinical and cost variation and the impact such initiatives might make on these populations.
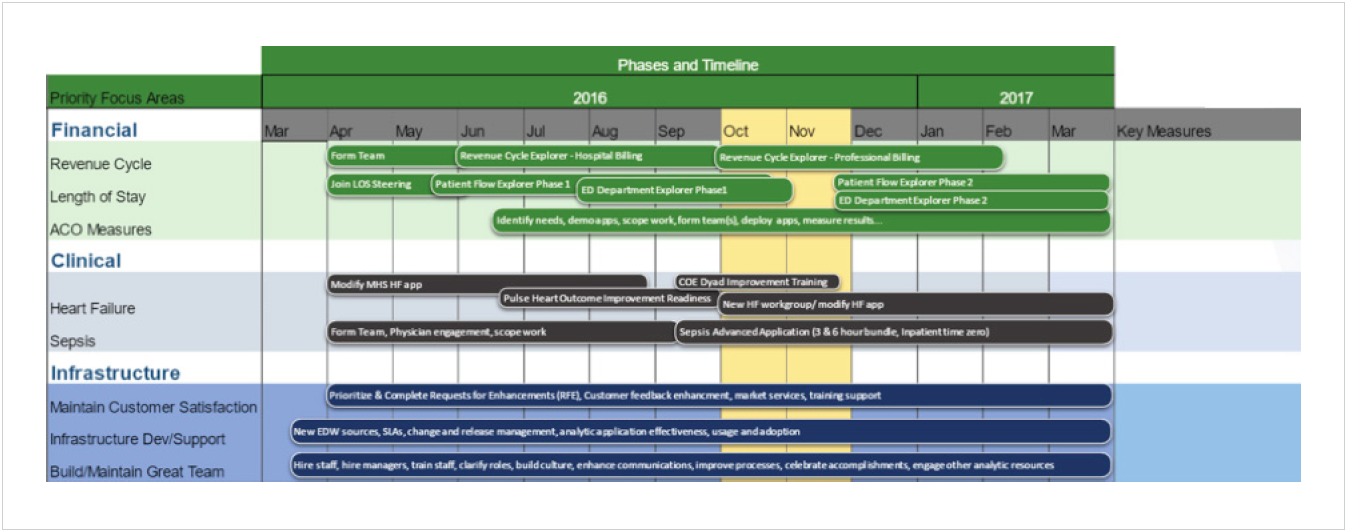
Between the readiness assessment and the opportunity analysis, MultiCare now had a common lens for understanding project load, maintenance, and analytics infrastructure work. Results helped to guide the development of the Shared Governance Committee’s prioritization process and strategic roadmap (see Figure 1).
Creating alignment. The need for alignment in a shared governance structure is necessary on many levels. The most obvious is aligning on a standard quality improvement methodology, along with a consistent framework for outcomes improvements that can be used throughout the health system. At MultiCare, the standard improvement methodology in use across the organization is a combination of Lean/6 Sigma, with an emphasis on the Plan-Do-Check-Adjust (PDCA) cycle approach.
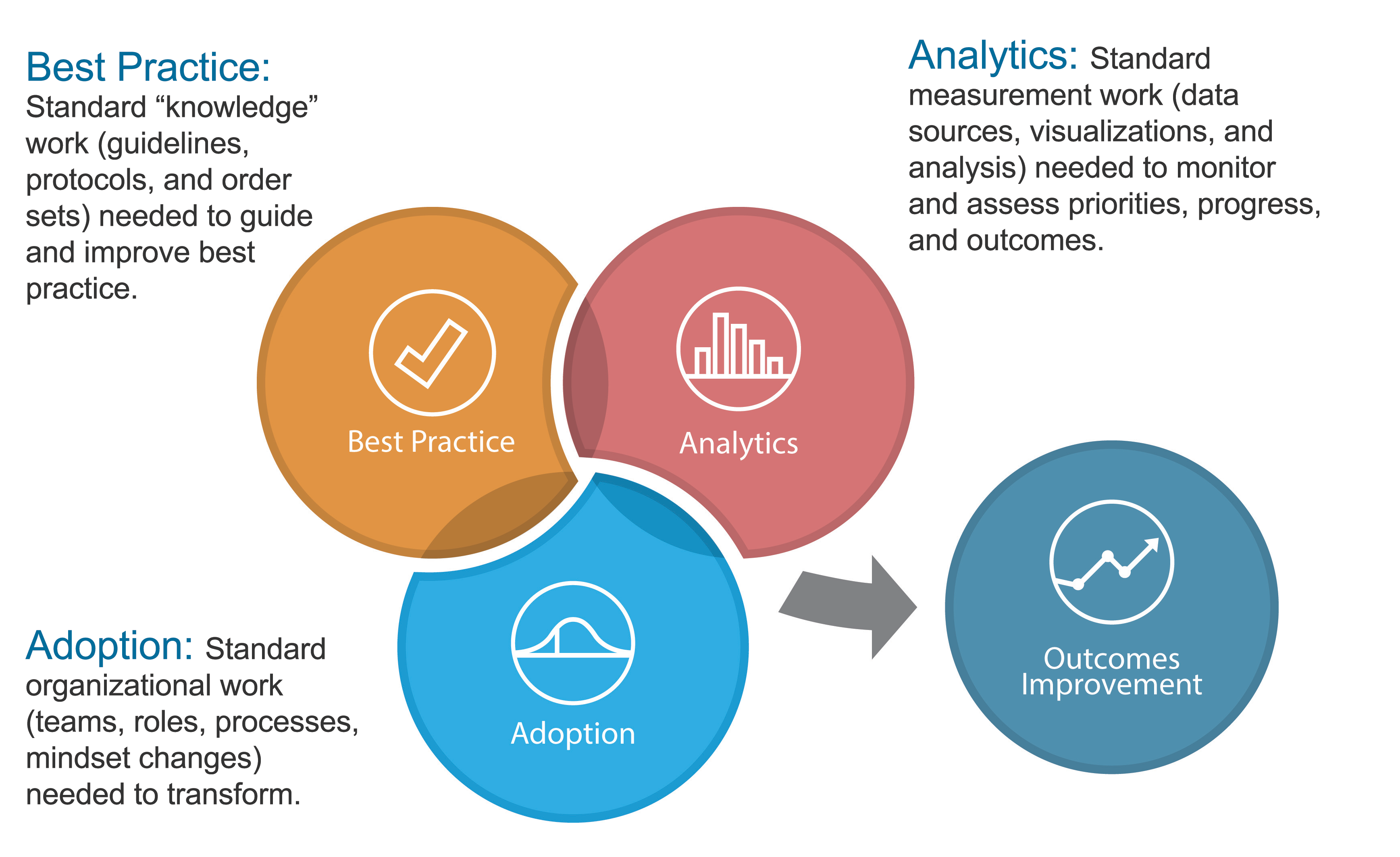
MultiCare had also adopted the Health Catalyst three systems framework (see Figure 2), which describes the components of successful outcomes improvement work in healthcare organizations as a balance of expertise in best practice, adoption, and analytics. Without all three systems in place, organizations struggle to create and sustain repeatable improvements. MultiCare had adopted this framework years before when it established its Collaborative program structure for quality improvement. The framework and the Collaborative structure were so successful that MultiCare brought both into its new governance structure. Through the addition of the Shared Governance Committee, the Collaboratives gained greater alignment with the overall MultiCare systemwide goals, objectives, and improvement efforts.
Aligning incentives is also necessary, including aligning the at-risk incentives of the MultiCare and Health Catalyst partnership with the overall strategic objectives of the MultiCare board and executive leadership team. The same MultiCare key strategic objectives were cascaded through its leadership structure using its leader evaluation management tool. Each year every leader selects individual goals that support the achievement of these overall strategic objectives that are tied to performance incentives. This approach creates common, synergistic goals throughout the organization.
Focus. The Shared Governance Committee next turned its attention to establishing processes that would effectively prioritize which improvement initiatives to take on. Here the team established a set of prioritization principles to guide and provide consistency. When setting its annual priorities to meet board approved systemwide goals, each potential improvement initiative is evaluated to see if it supports MultiCare’s strategic priorities as identified by the governance committee, and if it is directly reflected in the annual bonus framework. The committee also balances the portfolio of initiatives to make sure that the combination supports the three major categories of improvement:
Additional requests are prioritized according to an agreed upon prioritization criteria and available resource capacity, using data and analytics to guide decisions whenever possible. The prioritization process is designed to empower MultiCare’s resources to act on the best available information and guiding principles, saying “no” to out of scope requests, and avoiding bottlenecks. While the process is designed and implemented to yield those results, it is not yet fully effective, but clearly heading in that direction. To further integrate the prioritization process, maintain alignment, and build a shared understanding, MultiCare is trying to consistently provide transparent communication early and often into key priorities, capacity, initiatives, and timeliness.
Once projects are prioritized, the Shared Governance Committee determines the allocation of available analytic resources among the three categories of improvement: clinical, financial, and analytic infrastructure. Once these high-level decisions are made, the categorical allocation is distributed among the improvement initiatives in that category by those closer to the work. For example, each Collaborative receives an allocation of analyst hours to support its improvement work. The amount allocated was part of the original chartering process for these groups. It is then the responsibility of the Collaborative to determine how to use the analyst time to support the multiple improvement projects sponsored by that Collaborative.
Another example is the Pulse Heart Institute (PHI), which is responsible for six centers of excellence and their associated improvement work. Prior to the Shared Governance Committee making their allocation decisions, the leaders of the PHI made a presentation to the committee detailing the work that they wanted to pursue and the expected costs and benefits. This information was taken into consideration when priorities were set and used to determine the level of analytics resources allocated to the PHI. The PHI leadership will determine how those resources are distributed among their six centers of excellence.
In addition to the allocated time of internal analysts, access to specialized analytics resources from Health Catalyst is also available for prioritized improvement projects. This creates the opportunity to utilize additional expertise in areas such as machine learning, which can be used to develop risk models and predictive tools for decision support that can then be incorporated into the analytics applications and workflow.
To make sure that hard-won gains in outcomes improvement are not lost when other projects are started, MultiCare has implemented a performance excellence dashboard that is readily accessible and frequently updated. Effective use of this dashboard allows teams to launch new initiatives while monitoring ongoing performance of previous efforts.
The dashboard shows the performance on organizational strategic objectives through systemwide outcomes measures (e.g. readmissions, mortality, and length of stay). Metrics can also be filtered by specific cohorts where improvement efforts have been focused such as acute myocardial infarction, heart failure (HF), or pneumonia, thus providing feedback on individual improvement initiatives. By monitoring this dashboard, the Shared Governance Committee, executives, department leaders, and individual improvement teams can identify when performance slips in a particular area, even if the improvement team is no longer active. This allows the appropriate stakeholder to re-engage a team when needed, or inform an existing team of a change in performance that needs attention, and quickly initiate action to uncover and fix the underlying issue.
Establishing the Health Catalyst partnership and implementing a governance framework has allowed MultiCare to move forward with confidence in its journey to becoming a data-driven organization focused on improving the health of its patients and community. Today, MultiCare is better able to mobilize its organization and accelerate its achievement of excellence in clinical and financial outcomes, service, and access. As such, the health system plans to incorporate more benchmarking and machine learning into its processes and analysis, and eventually into decision support from the bedside to the board room.
Ultimately, MultiCare seeks to be a lifelong learner—and teacher. Partnering with Health Catalyst, who works with many different types of healthcare organizations, enables MultiCare to learn and to share best practices with others.