Mission Health's trauma services focus on evidence-based patient care but faced challenges in timely monitoring key process measures due to the manual data review burden. To enhance trauma care, the organization implemented data and analytics for quick insights into injury-specific performance and concurrent chart reviews.
Complex trauma systems require several individual processes to facilitate evidence-based patient care. The success of a trauma program's effectiveness in delivering high-quality patient care relies on the ability to continuously monitor process measures.
North Carolina’s Mission Health trauma services provide evidence-based care. Despite its efforts to measure the impact of this care on outcomes, the overwhelming burden of manual data review limited its ability to effectively monitor key process measures in a timely manner. This prompted Mission to use data and analytics for timely insights into injury-specific process measure performance and concurrent chart review to improve trauma care.
Trauma systems are complex, requiring many individual processes to facilitate evidence-based patient care. Ongoing monitoring of process measures is key to evaluating trauma program effectiveness in delivering high-quality patient care.1
One of the nation’s leading providers of healthcare services, HCA Healthcare is made up of locally managed facilities that include 185 hospitals and 119 freestanding surgery centers located in 21 U.S. states and in the United Kingdom. Mission Health, an operating division of HCA, based in Asheville, North Carolina, is the state’s sixth-largest health system and includes six hospitals, numerous outpatient and surgery centers, post-acute care provider CarePartners, and the long-term acute care provider Asheville Specialty Hospital. It also has the region’s only dedicated Level II trauma center, Mission Hospital, which provides care to over 3,500 trauma registry patients annually. The organization sought to ensure the quality of its trauma systems.
Mission trauma services provide evidence-based care. Despite best efforts to measure the impact of the evidence-based care on outcomes, the overwhelming burden of manual data review limited the organization’s ability to effectively monitor compliance with key process measures in a timely fashion.
Access to data was delayed up to six months. The available trauma registry data was pulled from different sources, each with different definitions, requiring manual processes to discern the true meaning of the data, making concurrent case review difficult. The disparity in data definitions led to unclear expectations and inaccuracies or omissions in the documentation of grade/level of a spleen injury, impacting the decision process for definitive treatment.
Pain management after a rib fracture varied widely by clinicians, resulting in some patients with rib fractures developing ineffective breathing patterns, requiring transfer to critical care for airway management and possible intubation.
Mission desired a data-driven solution for improving trauma care and gaining timely insight into injury-specific process measure performance. The organization needed to perform concurrent chart reviews, allowing program leaders to provide feedback to clinicians, and drive adoption of the evidence-based care that results in the best possible patient outcomes.
Mission relies on care process models (CPMs) to decrease variation and standardize care throughout the organization, ensuring patients receive evidence-based best practice, patient-centered care, delivered in the right care setting at the lowest cost to patients. The CPM for patients with traumatic injuries involves interventions and process measures to drive care from the point of presentation to discharge, including for patients admitted to inpatient care.
The CPM for patients with spleen injury was developed to guide clinicians in assigning accurate grade/level of spleen injury and the standard documentation required. Clear understanding of the grade/level of injury supports better decision-making for managing the patient’s treatment, including non-operative, interventional radiology, or operative management.
As a data-driven organization, Mission leverages the Health Catalyst® Data Operating System (DOS™) and a robust suite of analytics applications, including the Trauma Advanced Analytics Accelerator, to gain insight into trauma injury data. The analytics accelerator allows the trauma program team to review injury-specific trauma data, enabling concurrent review of trends in care delivery, and timely evaluation of patient outcomes. Mission can efficiently review patterns of injury, compliance with different CPMs, adherence to CPM interventions and process measures, and can compare the outcomes of patients who have received these interventions with those who have not.
Using the analytics accelerator and robust trauma program data, the Mission trauma program team was able to effectively and efficiently analyze the volume of patients with spleen injuries, and the various grade/level of injury (see Figure 1).
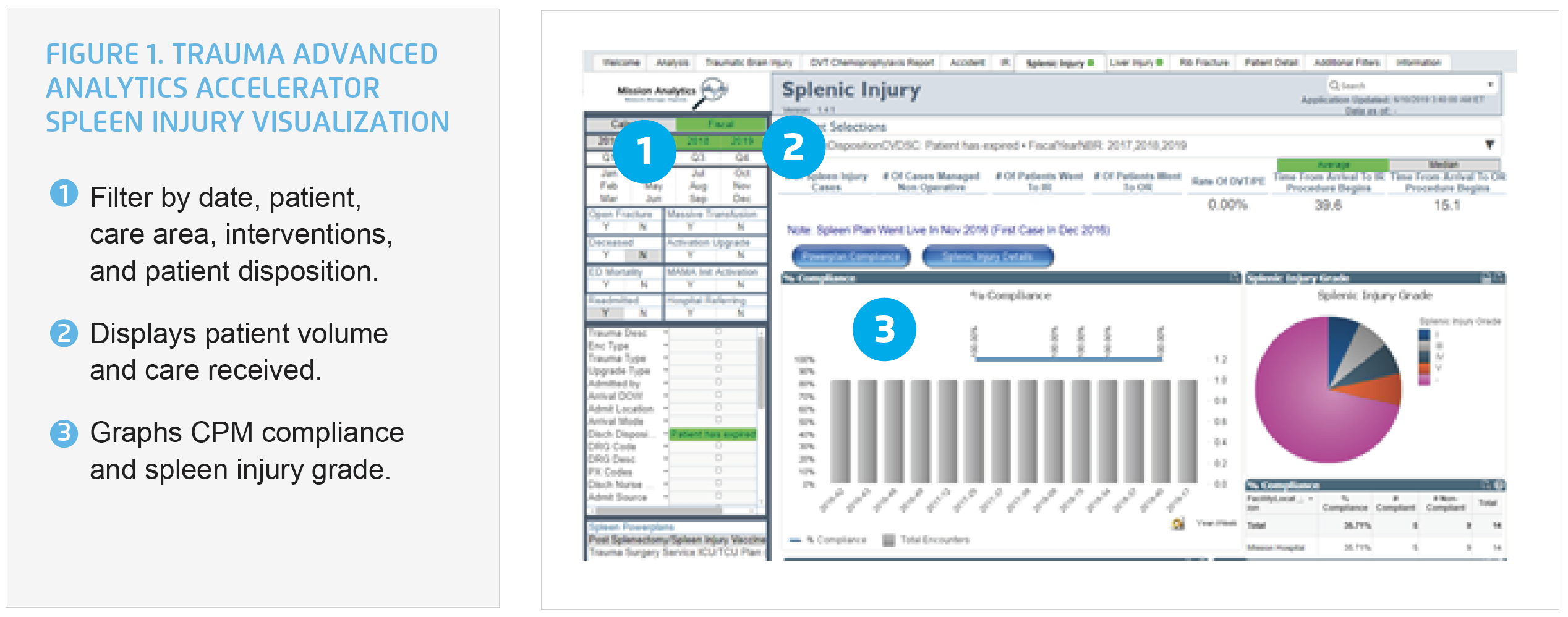
The trauma program can complete concurrent case review, using the data from the analytics accelerator to advance the adoption of the CPM for patients with spleen injury, increasing the number of patients who receive the most appropriate evidence-based interventions. The trauma program can offer both aggregate and individual performance data to individual clinicians, identifying opportunities to improve, and sharing feedback about positive performance. Data is shared with clinicians in peer to peer conversations, and during department meetings.
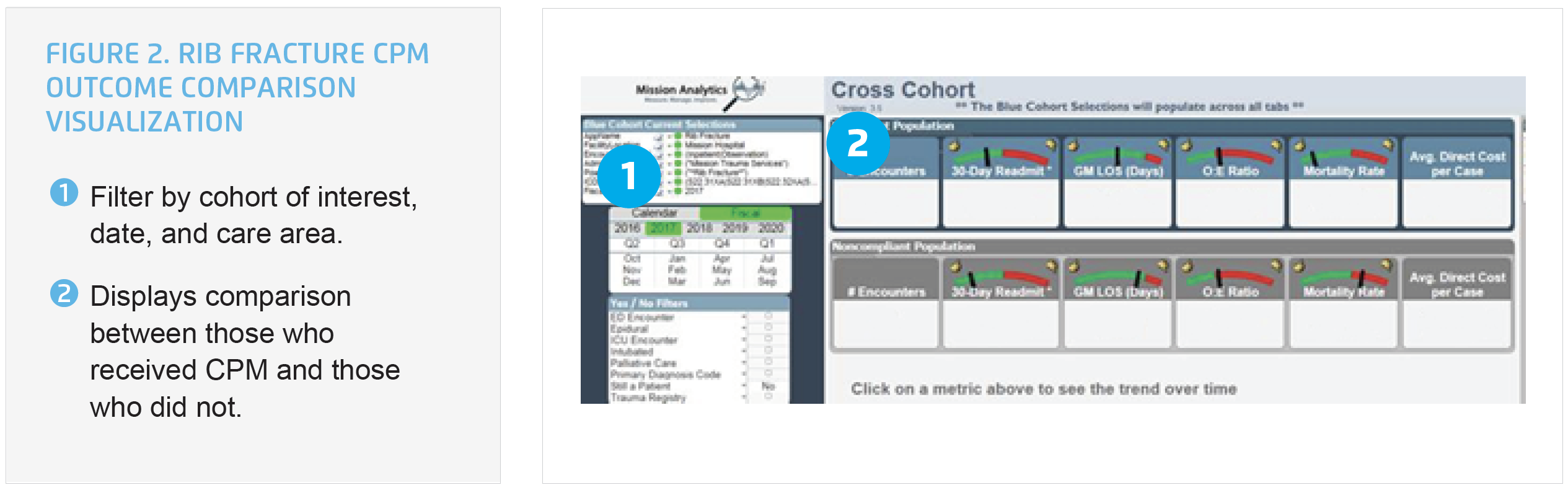
Individual clinicians are provided access to the analytics accelerator, and receive education on how to use this tool, enabling ongoing self-assessment. The trauma program is also able to use the analytics accelerator to gain insight into compliance with the CPM for pain management for patients with a rib fracture and evaluate the impact of the CPM on patient outcomes. The difference in outcomes can be visualized between patients who received the rib fracture CPM with those who did not and can demonstrate the value of using the CPMs to their teams (see Figure 2).
Using this data-driven approach, Mission has achieved meaningful improvements in the care of patients with rib fractures and spleen injuries, including:
Patients with spleen injury:
Patients with rib fracture injury:
“We can now look at injuries and identify information that pinpoints trends. The ability to peel back layers is powerful. We can look at groups and subgroups with the ability to do things we could only dream about 12 months ago.”
– William Shillinglaw, DO Medical Director Trauma/ Critical Care Services, Mission Hospitals
Mission intends to extend its data-driven process to support the implementation of its aggressive deep vein thrombosis prophylaxis protocol for patients with traumatic injury. The organization also plans to use the analytics accelerator for ongoing monitoring of performance, and comprehensive evaluation of patient outcomes.