In the U.S., nearly one in three women give birth via cesarean delivery. Unnecessary cesarean deliveries can expose mothers and babies to possible harm without providing many benefits. Read how Gunnison Valley Hospital reduced the number of unnecessary cesarean deliveries by standardizing labor and delivery care practices and utilizing data from its analytics platform.
In the U.S., nearly one in three women give birth via cesarean delivery. Rates vary widely by state, ranging from a low of 23 percent to a high of nearly 40 percent. Despite the potential life-saving benefits of a cesarean, this large variation suggests that unnecessary cesarean deliveries are frequently performed and that potentially modifiable factors, such as patient preferences and practice variation among hospitals, systems, and healthcare providers, likely contribute to the high rate.
Gunnison Valley Hospital has a long history of safe obstetric care, delivering more than 150 babies annually, yet the rates of elective early induction (prior to 39 weeks gestation), primary cesarean, and Nulliparous, Term, Singleton, Vertex (NTSV) were somewhat higher than desired. With the help of analytics, Gunnison shined a light on its labor and delivery practices and developed standard procedures aimed at producing better outcomes for patients.
Nearly one in three women in the U.S. who give birth do so by cesarean delivery. Rates vary widely by state, ranging from a low of 23 percent to a high of nearly 40 percent. Cesarean birth can be lifesaving for the fetus, the mother, or both. Yet, a large variation in cesarean birth rates suggests that potentially modifiable factors, such as patient preferences and practice variation among hospitals, systems, and healthcare providers, likely contribute to the high rates of unnecessary cesarean deliveries.1
The NTSV cesarean birth rate—which identifies the proportion of live babies born at or beyond 37.0 weeks of gestation to women in their first pregnancy, that are singleton (no twins or beyond), and in the vertex presentation (no breech or transverse positions) via cesarean birth—is a meaningful obstetric quality measure, as variation in the NTSV cesarean delivery rate among providers suggests many hospitals may be able to safely improve their rates through quality improvement initiatives.2
A factor contributing to increased cesarean deliveries is the induction of labor before the cervix is “ready.” Current guidelines recommend elective induction not occur prior to 39 weeks, and after 39 weeks gestation, elective induction should only occur when the cervix is “ready” for labor, which is typically measured by using the Bishop score. Inductions, particularly when the cervix is not ready, carry risk, including increased risk of infection, uterine rupture, fetal death, and increased risk of cesarean delivery.3
Gunnison Valley Hospital is a critical access hospital located in Gunnison, Utah. The hospital has a long history of providing quality care with a wide range of services including family-centered labor and delivery services. Gunnison is committed to developing and maintaining trusted relationships with its patients and their loved ones through personalized care and cutting-edge technology; all while preserving a hometown atmosphere and familiarity.
Gunnison has a long history of safe obstetric care, delivering more than 150 babies annually. However, its rates of elective early induction (prior to 39 weeks gestation), primary cesarean, and NTSV were, somewhat higher than desired.
While Gunnison had access to data about its performance through monthly reports, the delay in the timeliness of data access and lack of specificity of the data, hindered performance improvement efforts. Additionally, physicians had limited access to data specific to their individual practice and performance, leaving them largely unaware of how their practice and performance—particularly data regarding use of the bishop score, elective early induction, and NTSV rates—compared to that of their peers.
At Gunnison, assessment of readiness for induction varied widely, as the hospital didn’t have a standard process in place. While protocols for induction existed, they were not incredibly detailed and did not result in standard practice. Additionally, expectations for standard documentation in the EMR by physicians and nursing staff were in need of improvement. To reduce the variation in labor and delivery care, Gunnison needed a data-driven quality improvement approach, allowing it to reduce elective early induction and decrease the NTSV rate while maintaining positive outcomes for newborns.
To improve its labor and delivery performance, Gunnison partnered with Health Catalyst, implementing the Health Catalyst® Data Operating System (DOS™) Platform and the Labor and Delivery Advanced Application. DOS combines the features of data warehousing, clinical data repositories, and health information exchanges in a single, common-sense technology platform.
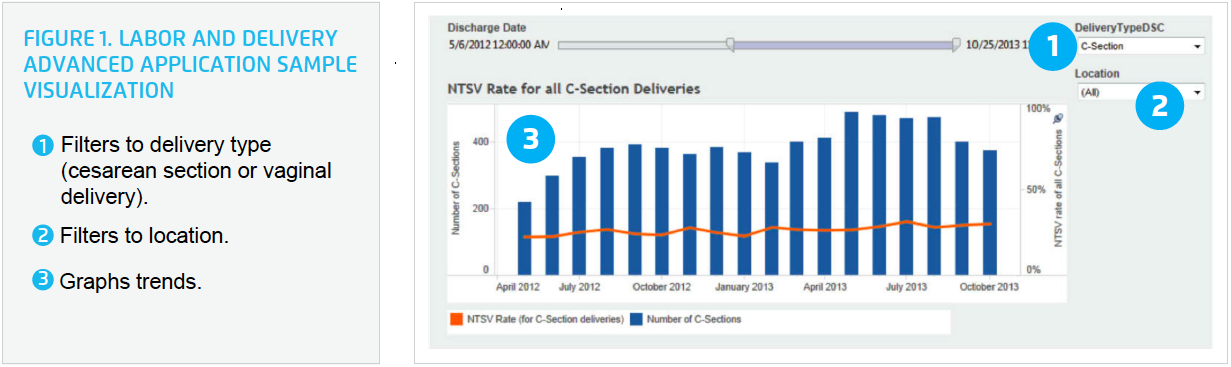
The Labor and Delivery Advanced Application supports clinical leaders, operational leaders, and quality improvement professionals with the data needed to support improvement efforts. The application provides visibility into the hospital system’s pregnancy cohort, aiding in the monitoring of performance and reporting of quality measures while helping to identify opportunities for improving care in elective early induction, primary cesarean, and NTSV rates (see Figure 1).
With improved access to meaningful, actionable data in place, Gunnison leaders identified that labor and delivery care could be improved, and convened an improvement team to support the effort. Members of the improvement team included a physician champion, members of nursing leadership, and a quality improvement specialist, all charged with identifying strategies to decrease variation in labor and delivery care.
Aware that elective early induction can lead to an increase in cesarean deliveries, the improvement team reviewed the available literature to identify best practices for induction. Using information from the literature, the improvement team updated Gunnison’s induction protocol to include a comprehensive favorable induction guideline that outlines:
The improvement team also developed and implemented a new standard workflow for scheduling inductions. Prior to scheduling, the clinic physician evaluates and documents the reasons for induction and relevant patient history. Upon patient arrival to the hospital, the admitting physician assesses and documents the Bishop score as a standard procedure.
To improve adoption of the induction protocol and standard workflow, Gunnison provided education to its physicians and nursing staff. The education outlined the importance of proper evaluation and documentation of cervical readiness using the Bishop score prior to induction and reviewed standard nursing labor management skills.
Gunnison developed a standard flowsheet within the EMR to help ensure consistency in documentation. Prior to building the flowsheet within the EMR, several small trials were conducted to ensure its effectiveness. Gunnison used the feedback from the trials to fine tune the documentation. The trials also allowed Gunnison to validate the desired documentation processes, while allowing the improvement team time to ensure data accuracy within the analytics application.
To further support improvement efforts, Gunnison recognized the need to integrate data in a way that equips providers and nursing staff with access to real-time, or near real-time, insights about performance, in addition to providing access to tools that can be used to improve practice. Using the analytics application, Gunnison is able to review physician-specific performance data, including elective induction rates, NTSV rates, and compliance with documentation of the Bishop score prior to induction.
On a quarterly basis, leaders use the analytics application to review performance on required documentation, including the consistency of pre-induction Bishop scores, and the resulting patient outcomes. Data from the analytics application is also shared at department meetings with the nursing staff and physicians. Physicians are given their specific performance data and information on how their performance compares to their peers. For many, this is the first time they have received their individual performance data.
Using this collaborative, data-driven approach, Gunnison successfully improved its labor and delivery care, resulting in:
Standardizing the processes used for elective early induction reduced both the NTSV and primary cesarean rate, as more women were “ready” for labor and able to have a successful vaginal delivery.
Gunnison accomplished these improvements while ensuring positive newborn outcomes, maintaining average newborn Apgar scores at one minute greater than seven, and Apgar scores at five minutes greater than eight.
“The ongoing focused education we provide for our nursing staff has given them more confidence in managing the laboring mother, further lowering the cesarean rate.”
– Brenda Bartholomew, RN, MSN, Chief Nursing Officer
Given the success of the labor and delivery care improvement project, Gunnison continues to use this approach to spread improvement processes to other patient populations. Next, Gunnison plans to improve the care provided to patients undergoing total joint replacement surgery.