An estimated one million cases of venous thromboembolism (VTE) occur each year in the United States—with approximately 300,000 of these cases resulting in death. Allina Health addressed VTE prevention and care by convening a physician-led workgroup standardized practices, leading to improvements in VTE bundle compliance, prophylaxis adherence, and discharge instructions for warfarin therapy.
Allina Health embarked on a three-year journey to address prevention and improved care for its Venous thromboembolism (VTE) patients—one of the most common causes of hospital-related death in the United States—and one of the most preventable.
Recognizing the need for standardizing best practices systemwide and creating a culture and infrastructure for continuous improvement, Allina implemented a physician-sponsored, multidisciplinary work-group to standardize order sets and engage clinicians in improvement efforts. The health system also implemented an enterprise data warehouse from Health Catalyst and a VTE analytics dashboard.
These efforts have resulted in measurable improvement in VTE prevention and care systemwide.
Venous thromboembolism (VTE) is a common, potentially lethal disorder that can result in long-term complications including pulmonary hypertension.1 Although the exact incidence of VTE is unknown, experts estimate that one million cases of the disorder occur in the United States each year, many of which represent recurrent disease.2 VTE occurs in both hospitalized and non-hospitalized patients, however, nearly two thirds of all VTE events result from hospitalization. A particularly sobering fact is that approximately 300,000 of these patients die.3 In fact, VTE-associated pulmonary embolism is the third most common cause of hospital-related death and the most common potentially preventable cause of hospital related death.4
Because of the prevalence of and risks associated with VTE, the Joint Commission (TJC) and the National Quality Forum developed six measures in 2005 to help care providers prevent and treat VTE. These measures were subsequently aligned with the Centers for Medicare & Medicaid Services (CMS) and became part of the CMS Inpatient Quality Reporting program.5
Allina Health, a not-for-profit health system dedicated to helping people live healthier lives in communities throughout Minnesota and western Wisconsin, committed itself to improving its processes for VTE prevention and treatment. The system—which consists of more than 26,000 employees, 5,000 affiliated and employed physicians, 13 hospitals, over 90 clinics, 16 pharmacies, and numerous specialty medical services—discovered excessive variation in its VTE processes across the enterprise. To reduce this variation and deliver on its brand promise that all patients would receive optimal care regardless of treatment location, Allina embarked on a three-year journey to improve VTE care.
Allina faced a significant challenge that all large health systems must overcome when integrating clinically across the enterprise: It had no systemwide standard practices in place to provide VTE prophylaxis or VTE follow-up care for the general inpatient medical population. The electronic health record (EHR) contained hundreds of order sets used when admitting patients, but no standard options existed for ordering VTE prophylaxis or for reminding providers when they failed to assess or order prophylaxis. In addition, Allina discovered that risk assessments for VTE existed in several forms and that clinicians did not apply them consistently across patients.
A lack of readily available data and easily repeatable analytics processes also served as a barrier for Allina to improve VTE care and meet CMS Core Measures. Health system leaders recognized they had limited access to high-quality data integrated from clinical, financial, and other source systems. For example, they could query frequency of prophylaxis orders, but they didn’t have a good process in place for understanding contraindications or the level of risk a patient faced for developing VTE. Furthermore, when patients developed VTE, the system had no way to track best practices in follow-up care.
As Allina embarked on its journey to promote optimal prevention and treatment of VTE, its goal was to identify and spread best practice throughout the enterprise while also improving the VTE Core Measure performance scores by incorporating best practice into provider workflow.
The health system began its improvement initiative by identifying a physician executive sponsor and establishing a physician sponsored, systemwide VTE workgroup. These leaders fostered a multi-disciplinary, highly collaborative process across clinical teams in the hospitals by involving clinicians (including nursing, pharmacy, and physicians), clinical decision support, business intelligence experts, education, analysts and enterprise reporting. Leaders achieved physician and staff engagement through involvement, transparency and education.
In addition to creating new organizational structures and engaging clinicians, Allina articulated a number of objectives, including:
The EDW aggregates clinical, financial, operational, patient satisfaction and other data to create consistent views of the data and to inform decisions. By automating the data-capture process—which involved creating structured data fields in the EHR to automatically capture and extract required data into the EDW—Allina has been able to move beyond its once highly-manual analytics process. This automation makes the method of capturing and communicating information and reporting to regulatory bodies significantly more efficient, which frees valuable resources to focus on using data to drive improvement.
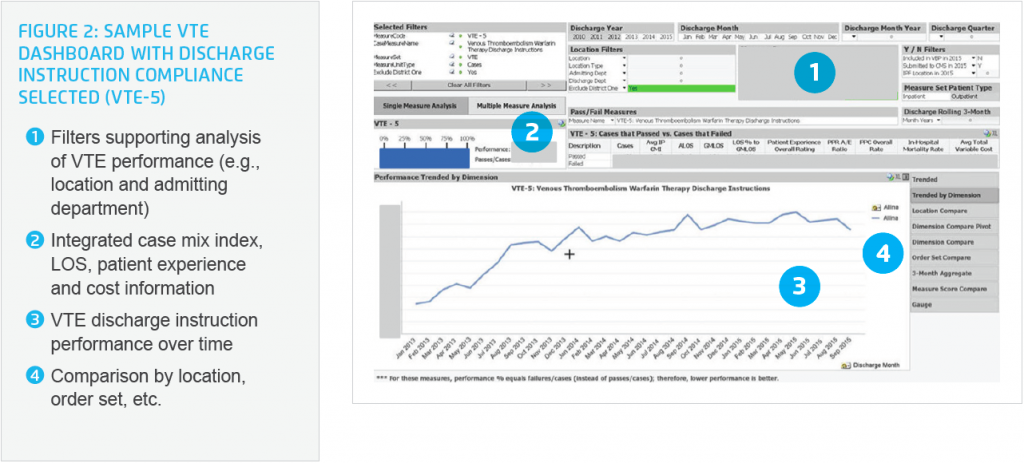
Allina also implemented a VTE dashboard (see Figure 2) to monitor and manage performance. This dashboard enables the team to identify target areas for improvement and to guide decisions in selecting and evaluating VTE prophylaxis and treatment tools. The dashboard also helps the team to drive behavior change and serves as a valuable case-finding tool. For example, it enables the team to identify groups of high-risk patients that may need more focused interventions for VTE prophylaxis.
Health system leaders engaged hospitals throughout the system to gain buy-in and participation in the initiative. For example, Allina engaged hospitals in identifying best practices. If one facility identified a best practice, leadership made a conscious effort to spread it across the entire system. In the midst of this drive for standardization, leadership still allowed each hospital to make slight modifications to the approach—as long as it delivered the same results. Where possible and appropriate, the team hardwired best practice into the EHR to promote consistency and optimal care, while also striving to avoid disrupting physician workflow or causing alert fatigue.
The combination of analytics and engagement efforts has resulted in measurable improvement in VTE prevention and care across Allina facilities. Key achievements include the following:
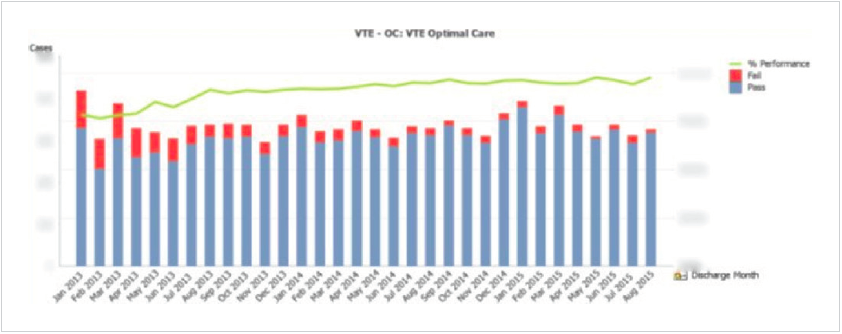
Allina increased its compliance with the VTE optimal care bundle by an absolute percentage of 19 percent – resulting in an actual compliance rate of 97 percent (see Figure 1). Leadership attributes this achievement to a combination of:
At the beginning of this initiative, Allina did not have a standard VTE risk assessment tool or order group to incorporate into established order sets. The team successfully incorporated a standard, systemwide, evidence-based VTE risk assessment tool and order group into Allina’s order sets with a hyperlink to the VTE guideline. This effort involved updating 308 order sets (including 26 general admission order sets). As a result, almost 100 percent of general admission order sets now contain the standard VTE order group. Most importantly, this effort required effective physician engagement to make the order sets clinically relevant and allow them to be incorporated seamlessly into physician workflow.
Through a combination of standard, evidence-based guidelines and decision support, Allina realized a 8 percent absolute increase in VTE prophylaxis provided to patients (or documentation of a reason why prophylaxis wasn’t given), resulting in 97.9 percent actual compliance. Providing access to high quality, trustworthy data in applications with filtering and drill-down capabilities was critical to physician engagement and this successful outcome.
Based on a best practice identified at one hospital, Allina made pharmacy personnel accountable for discharge instructions at all hospitals to improve performance and to relieve physicians and nurses of the responsibility. Allina leadership saw putting pharmacists in charge as fundamental for improvement on this metric. The system subsequently realized a 63 percent absolute increase in providing and documenting appropriate instructions for patients with confirmed VTE discharged on warfarin. This represented an actual compliance rate of 92.4 percent (see Figure 2).
“Continuously improving care for patients is foundational to who we are at Allina Health. This kind of improvement requires a comprehensive, multidisciplinary effort. It requires good data to identify improvement opportunities and analytics tools to track progress. It requires educating clinicians and staff along the way to ensure adoption of new processes and tools.”
– Michael Ornes, MD, Hospitalist, Allina Health
Allina will continue to focus on improving VTE care. It will especially turn its attention to measuring clinical outcomes such as rates of confirmed VTE and the clinical factors associated. The team will also continue to improve the VTE best practice advisories that aid in ordering and applying VTE prophylaxis as well as providing treatment to patients with VTE.


