After a turbulent 2020 and a 2021 the New York Times summed up as “languishing,” healthcare leaders are determined to pursue positive change in 2022. The pandemic still looms large, but health systems will also focus on other prominent performance drivers, following the lead of top performers in other industries that stress long-range tactics and prioritize consumers and data-driven decision making. With these strategies in place, trends in the following six areas will determine organizational success in 2022 and have a lasting impact on providers and patients:
1. Health equity.
2. Patient safety.
3. Staffing.
4. Care delivery.
5. COVID-19 recovery.
6. Payment and payers.
With the New York Times summing up the predominate feeling of 2021 as “languishing,” 2022 begins with a mix of uncertainty and concern but also optimism. Healthcare and society at large are eager for a positive post-pandemic future. Moving into this next phase, 2022 healthcare trends in six areas stand to shape healthcare delivery and policy and patient and provider experience moving forward: health equity, patient safety, staffing, care delivery, COVID 19, and payment and payers.
But what does “moving forward” mean on an industry level? If healthcare follows the lead of other sectors in to 2022 and beyond, leaders will stress long-range strategies (e.g., 10-year plans) that prioritize consumers and data-driven decision making.
Multinational beverage conglomerate Anheuser-Busch InBev (AB InBev), which projected growth between 10 and 12 percent in 2021 and continued expansion between 4 and 8 percent in 2022, is taking a consumer-centric value approach into 2022. AB InBev has stated a commitment to a “future with more cheers,” which the company describes as “a company-wide purpose to dream big about the future we want to shape and how we can do our part to realize it.”
The organization plans to realize this future by moving from a traditional growth strategy around cost management and generation and mergers-and-acquisitions (M&A)-driven growth to new consumer-centric approach. AB InBev’s revamped purpose focuses on superior value for customers, largely enabled through digital technology that will sell directly to the retailers and the consumers.
Other high-performing brands in 2021, according to the Drucker Institute ranking, include top-five companies Microsoft, Amazon, Apple, IBM, and Intel. These organizations have survived the pandemic well and share a commitment to innovation. Health Catalyst sees companies prioritize high-value data with the following understanding:
As healthcare organizations work to embrace some of the key drivers of success behind top-ranked brands, such as a consumer-centric approach and a commitment to high-value data, trends in six areas will differentiate the highest performing health systems from the rest.
In 2019, 25 percent of healthcare organizations rated health equity as one of their top priorities. In 2021, health equity rose to 58 percent, while other measured areas (safety, health, value, improvement, science, and joy in work) were relatively stable—placing equity as a frontrunner in industry priorities for 2022.
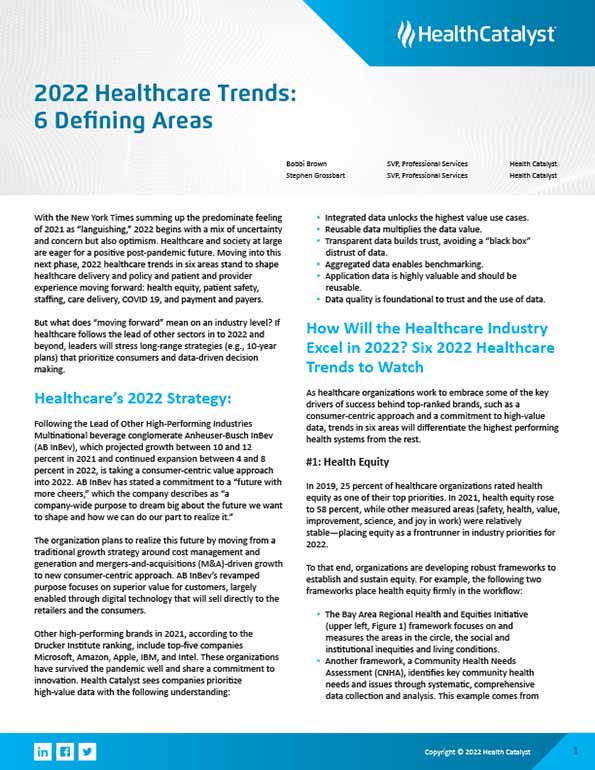
To that end, organizations are developing robust frameworks to establish and sustain equity. For example, the following two frameworks place health equity firmly in the workflow:
The above frameworks focus on understanding community needs—a key driver in health equity. And many organizations are making similar priorities. For example, more than 75 companies have signed the Digital Health Equity Pledge, an initiative by Executives for Health Innovation, to look as equity issues including accessibility, diversity, respect, and relevant public policy.
CMS has also joined healthcare leaders with a focus on health equity and is helping drive related trends. For example, in the finalized 2022 Inpatient Perspective Payment rule, CMS asks for comments from stakeholders on the potential future reporting on structural measures to assess hospital leadership engagement in health equity performance data. In other words, CMS has informed stakeholders that they’re going to assess how closely CEOs and other leaders look at health equity and use it to drive and improve performance. CMS will ultimately tie equity assessment into the payment systems that drive healthcare business.
Furthermore, CMS has already positioned data to support health equity prioritization. Like many payers, CMS supports using Z codes. Payers use these ICD-10-CM codes to document social determinants of health data (e.g., housing, food insecurity, and transportation) to understand community needs and opportunities for change.
On the organizational level, organizations can follow six action items around equity prioritization in 2022:
Significant shifts in care delivery in 2020 and 2021 will continue into 2022. Notably, the healthcare model moved outside the walls of the hospital and into virtual care settings, as facilities met capacity during COVID-19. In 2020, CMS issued a waiver for acute care at home, and as of fall 2021, approved 175 hospitals to provide at-home acute care.
The shift to at-home care appears to be gaining momentum. For example, early in 2022, major healthcare organizations, including Kaiser Permanente and Mayo Clinic, invested $110 million in a company called Medically Home, which facilitates and coordinates treatment for high-acuity patients in their homes.
The Advisory Board further supports the forecasted care delivery shift away from the hospital. The consulting firm predicts that between 2022 and 2027, outpatient knee surgery will expand from 6.5 to 36 percent of cases, 20 percent of the current outpatient medical visits will be virtual, and home-based hospital care will increase from 1 to 30 percent.
Consistent with the site-of-care shifts in 2020 and 2021 has been growth in the telehealth space. CMS waivers temporarily expanded telehealth services during COVID-19. While overall part B Medicare population care declined 11 percent in volume from 2019 to 2020, telehealth visits went from 840,000 to 53 million in that same period.
With digital technology and workflows rising among stakeholders (from payers to pharma), patient-centered care becomes more critical. Actions around care delivery in 2022 will center on engagement:
COVID-19 dramatically impacted patient safety and quality. By the fourth quarter of 2020, the number of hospital-acquired infections had increased—in particular central line-associated bloodstream infection (up 47 percent), catheter associated urinary tract infections (up almost 19 percent), and notable rises in ventilator-associated events, MRSA, and others.
The above increases make sense, as patients have been sicker during the pandemic, with more people on central lines, catheters, and ventilators. Concurrently, volumes have overwhelmed staff and lowered clinician-to-patient ratios. And with many people avoiding routine care, preventive appointments, such as cancer screenings, have declined. For example, breast cancer screening was down almost 91 percent from 2019 to 2020. To what extent COVID-19 undermined cancer prevention in 2020 remains to be seen but will likely impact healthcare in 2022.
As an aside, surgical-site infections have declined during the pandemic, in part due to the reduction in elective surgeries. Meanwhile, hospital-acquired Clostridioides difficile (C. diff) has also declined in conjunction with COVID-19, with a decrease in people admitted with community C. diff.
Moving forward, the United States has work ahead to bridge its safety and quality gaps—regardless of the pandemic. Relative to countries with similar socioeconomic status, the U.S. spends close to 17 percent of its gross domestic product on healthcare, which is nearly double what the rest of the industrial world spends. And at the same time, objective measures of quality are lower in the United States.
Moving the cost and quality dial in 2022 will require health systems to leverage data and analytics and an adaptive problem-solving approach. At the same time, organizations can take the following action around patient safety:
With COVID-19’s vast changes on the world overall and healthcare, the pandemic has reshaped many areas of society and the industry. With ongoing waves of variants and health systems still confronting capacity issues and predicted losses for hospitals in 2021 reaching $54 billion, COVID-19’s economic impact will shape healthcare through 2022 and beyond. The pandemic also drove an increase of almost 10 percent in national healthcare spending and a 36 percent increase in federal expenditures.
Looking forward into 2022, inflation is at 7 percent, the highest in 40 years. Meanwhile, M&A revenue was up 25 percent in 2021 from 2020, with more anticipated in 2022 Significant organizations, such as, Oracle, Cerner, and HCA are acquiring new entities while others are merging to accommodate new care delivery models, such as the growth in ambulatory surgery.
Hospital operating margins fell in 2021, with more losses predicted in 2022, while the CARES Act provided some relief to hospitals between 2020 and 2021—at least $70 billion. In Figure 2, from the Kaufman Hall December 2021 National Hospital Flash Report, the yellow bar shows operating margin with CARES Act dollars, and the blue bar is without CARES money. As the graph shows, margins are coming back but haven’t yet returned to pre-pandemic levels.

Another notable COVID-19 healthcare business impact has been the cost of not getting vaccinated. According to the Kaiser Family Foundation, insufficient vaccinations as of June through November 2021 cost U.S. hospitals almost $14 billion in waste—waste meaning hospitalizations that could have been avoided and the societal impact, lost work, lost family, and mortality related to not getting vaccinated.
Moving into 2022, healthcare can take the following actions to navigate COVID-19’s ongoing impact:
Healthcare is facing a crumbling workforce coming into 2022. September 2021 saw the highest quit rates among U.S. worker, with 4.4 million leaving their jobs. In healthcare, estimates say two in five nurses and one in four physicians want to exit the profession in the next two years.
At the same time, demand for healthcare workers is projected to grow by 45 percent between 2020 and 2030, forcing healthcare to evaluate its workforce supply strategy. Organizations must look closely at data-driven labor management to predict and manage labor needs and improve workforce experience.
Along with labor management, actions organizations can take around staffing in 2022 include the following:
On the payment and payers front, ACA enrollment has exceeded 14 million. CMS is reviewing its payment models, with no new models expected before 2023. Alternative payment models are stable, with Medicare Advantage and Medicaid growing.
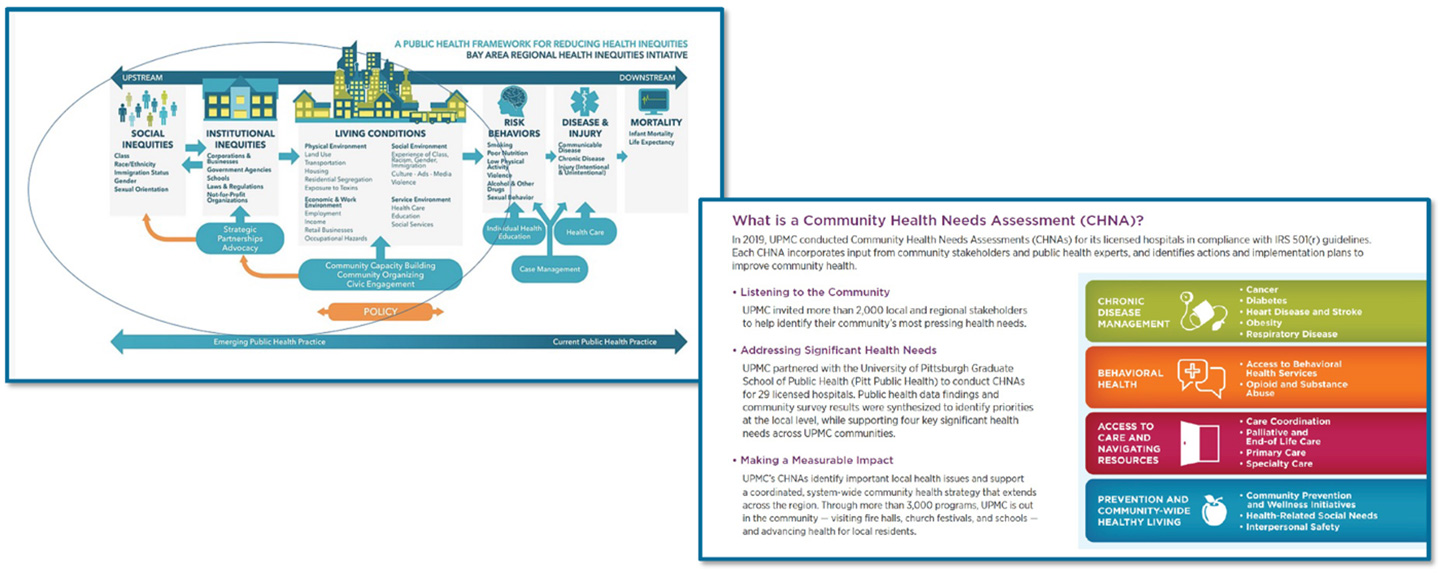
Organizations can expect to see CMS policy support five strategic objectives behind a health system that delivers equitable outcomes (Figure 3):
Additionally, CMS will make changes to measures, adjusting the way it calculates and uses some of its measures. For example, CMS is removing COVID-19 patients for quality measures and, in some cases, not basing dollars on pandemic-related events, such as pneumonia readmissions. CMS is also adding a reporting requirement for maternal health in 2022 to encourage hospitals to participate in collaborative programs to improve maternal outcomes.
With healthcare costs remaining high, leaders can anticipate that CMS will continue or expand its review of data and linkage to quality-based payments. CMS will continue down the path towards value-based care, increased affordability, and reduced spending. A notable shift for 2022 will embedding health equity in these efforts, per the strategic objectives in Figure 3.
Payers appear to be working closely with providers to best serve their communities. Such consumer-centric approaches include legislation around price transparency, such as the No Surprise Act, which took effect January 2022. CMS will also continue to enforce penalties for price transparency violations (i.e., organizations that don’t publish all their services and costs by mid 2022).
Health systems can navigate the 2022 payment and payer landscape by taking the following actions:
While languishing was a tough diagnosis to close 2021, the healthcare industry has a clear path for a thriving 2022. Trends in health equity, patient safety and quality, care delivery, COVID-19 response, staffing, and payers and payment are positioned to support continued recovery, rebuilding, and growth across the industry. Furthermore, as healthcare follows the lead of top performers in other industries with a long-range, consumer-centric, strategy the prioritizes high-value data, patients and providers stand to benefit from improved outcomes and better experiences.
Would you like to learn more about this topic? Here are some articles we suggest: