To stay in sync with healthcare’s transition to value-based care, payers today must develop the analytics capability to support alternative payment models and drive more value to their members. Payers can follow an analytics roadmap to develop a strategy that extends their data, analytics, and risk management expertise to meet growing demands.
The analytics roadmap helps the payer meet these common challenges of establishing a data-driven culture:
1. Recruiting and retaining high-quality providers in a competitive market.
2. Managing increasing numbers of high-risk/high-cost members with limited resources.
3. Efficiently reacting to federal and state legislative and payment changes.
4. Controlling the rising costs of healthcare services and pharmaceuticals.
As the healthcare industry continues to transition to value-based care (VBC) models, financial risk is shifting away from the payers and toward the providers. Payers are looking to alternate payment models (APMs) and other strategies to drive more value to their members.
To succeed in an environment of shared risk, payers must extend their data, analytics, and risk management expertise beyond their own walls. This article explains this extended approach to healthcare payer analytics and the value of developing an analytics roadmap for payers in the context of managing risk.
The first step in building an analytics strategy is to accept as guiding principle the words of W. Edwards Deming, “Without data you’re just a person with an opinion,” and make data an organizational imperative. The second step is to build a roadmap that leads to a data-driven culture. When payer organizations arrive at the data-driven destination, teams use analytics to identify opportunities and implement solutions to support new strategies, (e.g. enabling their providers to succeed in shared risk). Data drives decisions and actions.
By following an analytics roadmap, the payer organization will mature its use and understanding of data from traditional descriptive reporting to advanced predictive analytics. This transformation augments human intelligence, and providers and members can directly leverage its benefits:
A roadmap will help the payer navigate their own way through a minefield of potential risks associated with these challenges:
The well navigated data-driven journey through the minefield of risks will produce meaningful benefits, including the following six outcomes:
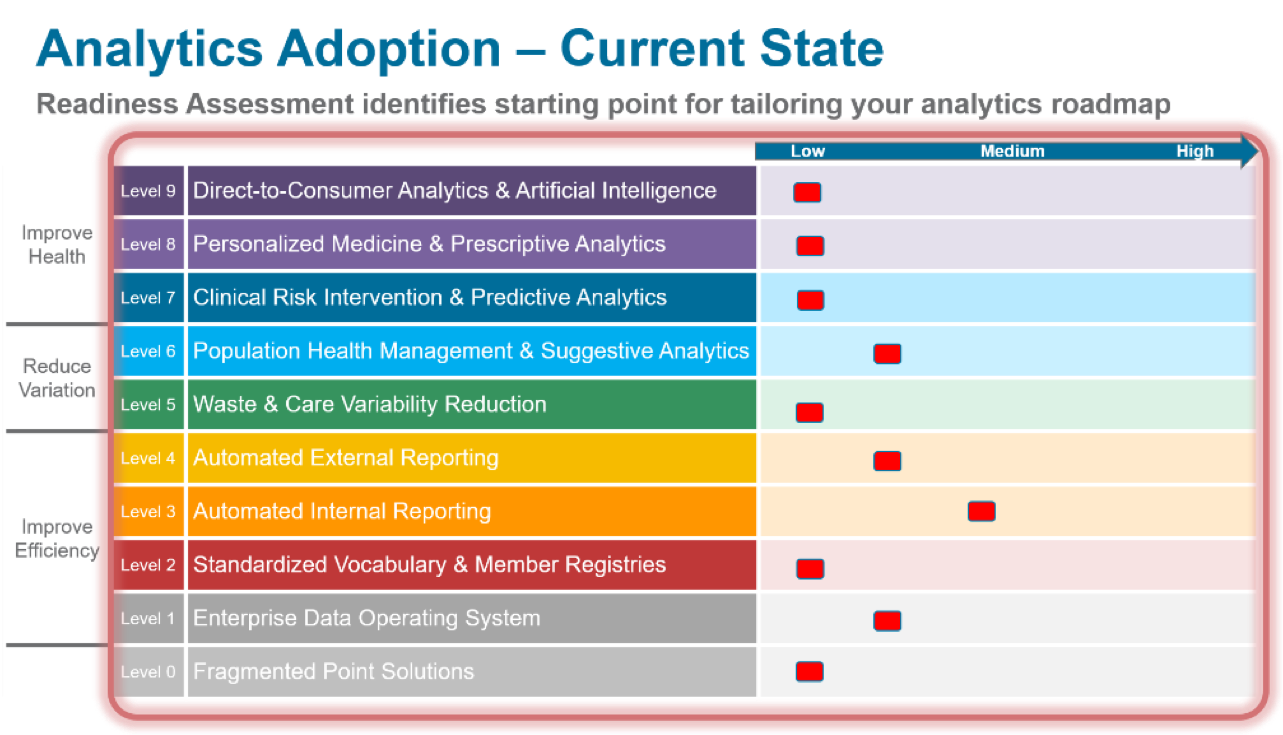
In the journey towards a data-driven culture, payers may partner with an analytics vendor or go it alone. Either way, an organization should use the Healthcare Analytics Adoption Model (Figure 1) as the context for a tailored analytics roadmap that progresses from a pre-enterprise data operating system to democratized data and, finally, to a data-driven cultures.

The pre-enterprise data operating system culture of spreadsheet silos, or pockets of analysis, generates conflicting reports and conflicting interpretations of data. This encourages battles over data ownership, long report request queues for consumers, and analysts spending most of their time hunting for and gathering data. The focus is on getting the right data and getting the data right (i.e., data completeness and the data accuracy).
The democratized data culture automates routine reporting and leverages a single source of curated data for ad hoc analysis. Governance teams spend significant time standardizing definitions and prioritizing data acquisition. The organization begins to trust the data, and report queues are significantly reduced with the availability of self-service applications and analyst-generated member registries.
When payer organizations arrive at the data-driven destination, they use analytics to identify opportunities and implement solutions to support new strategies (e.g., enabling their providers to succeed in shared risk). Data drives decisions and actions. The focus is on leveraging suggestive and predictive analytics to augment the move toward VBC and population health management.
As organizations mature in the use of data, they move from levels zero to nine (from fragmented point solutions to direct-to-consumer analytics and artificial intelligence) and progress through three key improvement categories:
Interestingly, as the organization matures its analytics adoption, it can reallocate human resources from lower levels, where they’re spending time on automatable tasks, to higher levels of analytic tasks. This allows its workforce to better apply its expertise (i.e., work at the top of their licenses), which reduces turnover.
Before adopting and executing an analytics roadmap, a payer organization should complete an analytics readiness assessment. The assessment identifies where an organization falls along the analytics adoption model—where it stands compared to industry standards—and ensures organizational expectations are in line with organizational capabilities.
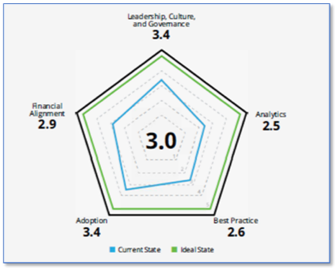
An analytics partner should provide an analytics readiness assessment. Health Catalyst, for example, offers an analytics readiness assessment with three components:
An organizational self-assessment identifies the detail behind the scores with key data consumers and/or consumer groups; this data informs one-on-one interviews focused on the above areas.

The results of the analytics readiness assessment (Figure 4) give the organization a readiness score (low, medium, or high), recommendations for improving analytics readiness, and the starting point for a customized analytics roadmap for that organization in the context of the Healthcare Analytics Adoption Model.
The readiness assessment also generates a list of short-term and long-term recommendations in three categories to tailor the route on an organization’s analytics roadmap:
The good news is that benefits begin accruing as soon as the organization executes the readiness assessment. Value builds through each phase of analytics maturity:
The analytics readiness assessment aims to help organizations determine if their analytics capacity is adequate and appropriate for succeeding in tomorrow’s healthcare environment. VBC models will mature as the inevitable context for addressing the rising costs of healthcare, and payers that mature their analytics capabilities in sync with the changes in the market will thrive.
Would you like to learn more about this topic? Here are some articles we suggest: