According to a November 2019 survey, 62 percent of clinicians and other healthcare professionals view burnout as a major problem industrywide. When asked for the best way to address clinician burnout problems, the most popular solution was less-complex workflows, which is the aim of emerging point-of-care analytics solutions.
Responses to additional questions reveal more about clinician burnout experience and views on the technology designed to help:
1. At your organization, how big of a problem is clinician burnout?
2. What is the best way to solve clinician burnout problems?
3. What are the biggest barriers to adopting closed-loop, point-of-care analytics capabilities at your organization
4. What are the biggest problems arising from a lack of adopting closed-loop, point-of-care analytics capabilities?

Almost half of clinicians today experience burnout—more than 40 percent of clinicians overall and 50 percent of female clinicians—according to a 2019 report, and many cite the EHR as a large contributor to burnout. But with billions of healthcare industry dollars invested in electronic systems and population and precision health models demanding increasing digitization, the EHR is here to stay.
With no perceivable way around healthcare digitization, one of the industry’s most pressing challenges is how optimize the clinician–technology relationship. How can data and analytics platforms help clinicians work better, not harder?
In November 2019 Health Catalyst surveyed clinicians and other healthcare professionals to learning more about professional burnout and how technology can help. A critical step, according to industry feedback, is more attention to clinician and other healthcare professional experience with and understanding of digital solutions—targeting messaging, education, and services around what healthcare end users need, when they need it.
Outcomes improvement companies have legitimate solutions to improve the accessibility and effectiveness of the EHR experience. For example, the Health Catalyst® Closed-Loop Analytics™ service aggregates data into customized workflows within the EHR or optimizes existing workflows for more effective calls to action for end users.
These emerging point-of-care analytics services are addressing clinicians’ top concerns around professional burden and dissatisfaction. For example, in the November 2019 survey, clinicians chose less-complex workflows as the number one way to solve burnout. The Health Catalyst Closed-Loop Analytics service make reliable, actionable data accessible at the patient bedside, allowing clinicians to perform the same functions within the EHR with six times fewer clicks, reducing time behind a computer and increasing time with patients.
If the solutions for clinician burnout aren’t clear to end uses, the problem certainly is. The majority (76 percent) of participants reported that, at their organizations, clinician burnout was a major or moderate a problem, and an overwhelming 95 percent said the clinician burnout was major to moderate problem industrywide. With research linking clinician burnout to depression and suicide—as well as twofold increased risk unsafe care, unprofessional behaviors, and low patient satisfaction—provider dissatisfaction is an urgent issue across healthcare.
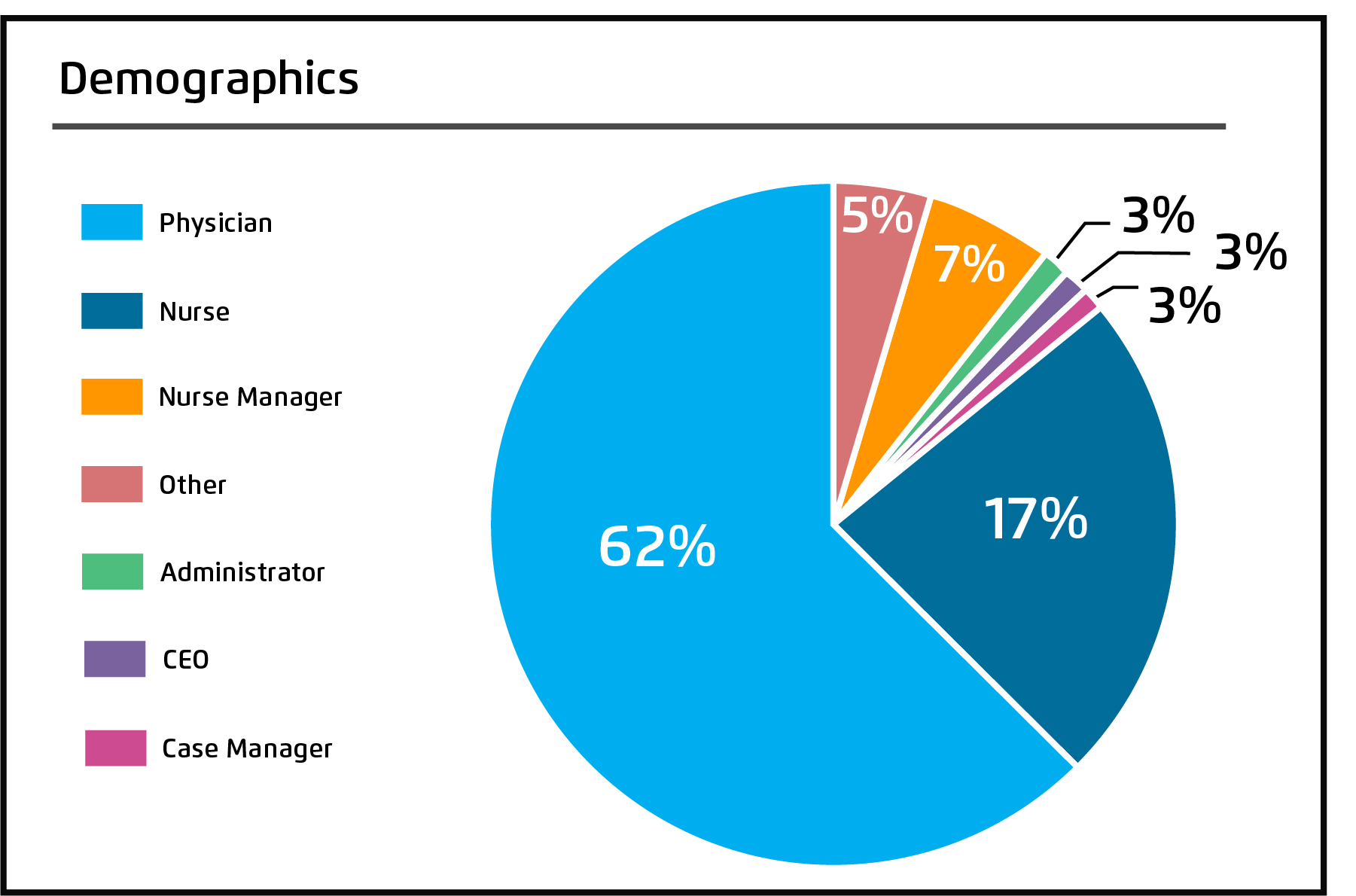
Of the 136 respondents to the Health Catalyst clinician burnout survey, 62 percent were physicians, 17 percent were nurses, and the remainder included nurse managers, case managers, healthcare administrators and CEOs, and more (Figure 1).
Participants shared their perspectives on the following questions regarding clinician burnout and how a closed-loop analytics solution affects them and their organizations:
#1: At your organization, how big of a problem is clinician burnout?
#2: For the entire healthcare industry, how big of a problem is clinician burnout?
#3: What is the best way to solve clinician burnout problems (Figure 2)?

Those who chose “other” added the following responses, indicating a desire to make care delivery more about the patient and less and data entry and requirements:
#4: What are the biggest barriers to adopting closed-loop, point-of-care analytics capabilities at your organization?
Respondents who selected “other” wanted to prioritize clinical care and judgment, see more appropriate data use, and have technology deliver better on its promises:
#5: What are the biggest problems arising from a lack of adopting closed-loop, point-of-care analytics capabilities (Figure 3)?
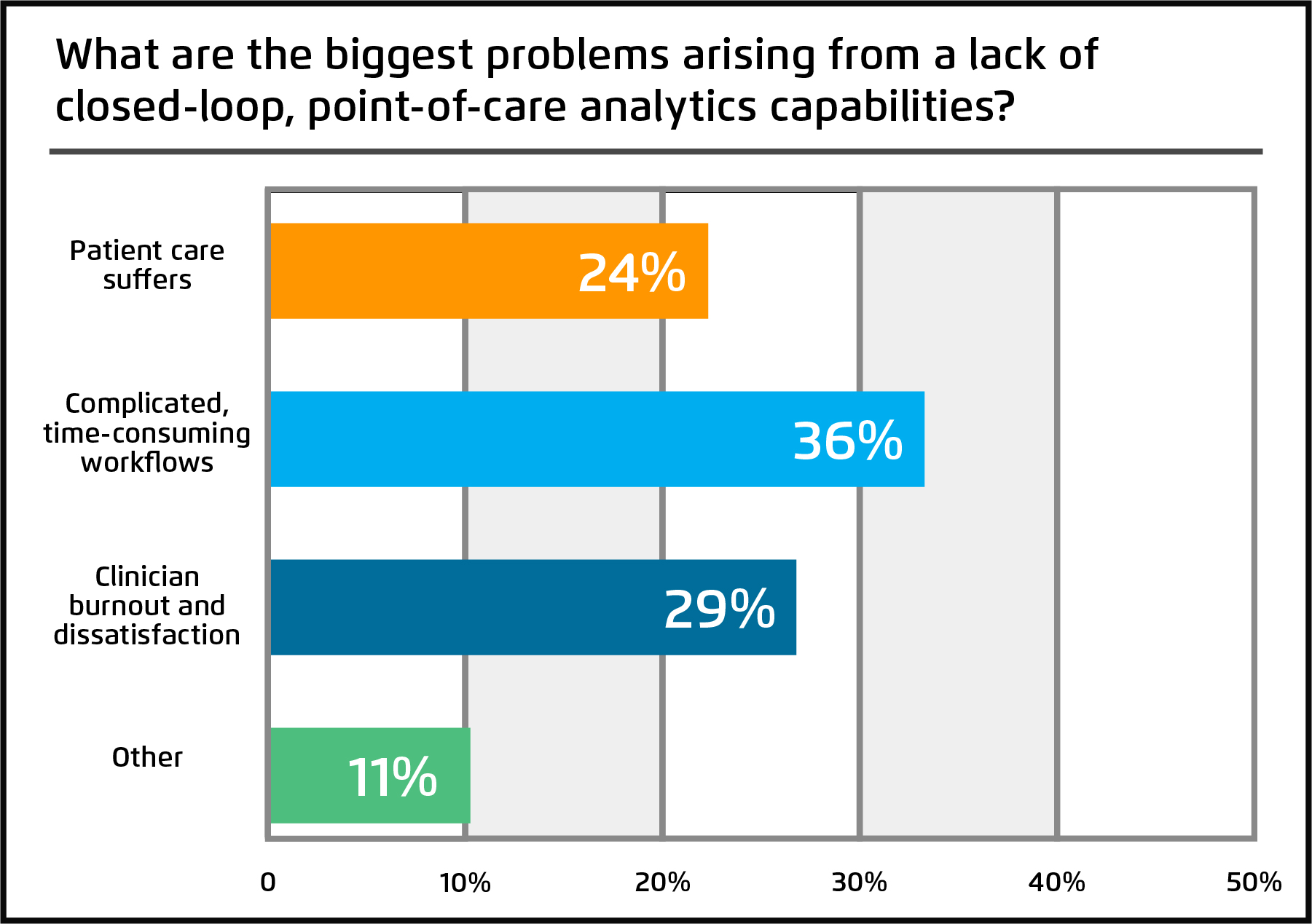
According to participant feedback on “other,” clinicians see the solution not as purely technological but as restructuring the processes and pressures preventing them from practicing at the top of their licenses:
#6: When is your organization targeting the adoption of data integration and workflow optimization via closed-loop, point-of-care analytics?
Clinicians often agree on two issues: clinician burnout is a significant problem for the healthcare industry, and they need less-complex workflows that minimize screen time and maximize patient interaction while helping the make the most informed decisions.
With a large portion of survey respondents viewing clinician burnout as a major problem, the industry is clearly ready for transformation. Successfully reducing clinician burnout and improving provider job satisfaction won’t come with faster, more agile analytics alone. To truly transform, next-generation workflow tools must cater to the needs and concerns of their end users with accessible platforms that enhance clinicians’ ability to deliver the best care according to their training and professional judgment.
Would you like to learn more about this topic? Here are some articles we suggest: