As health systems strive for financial growth and stability in a pandemic and shifting healthcare market, leaders often overlook a key opportunity to maximize profit margins for services rendered—a charge capture audit. A charge capture audit takes a deep dive into the charge capture process, exposing root causes of costly errors and suboptimal processes.
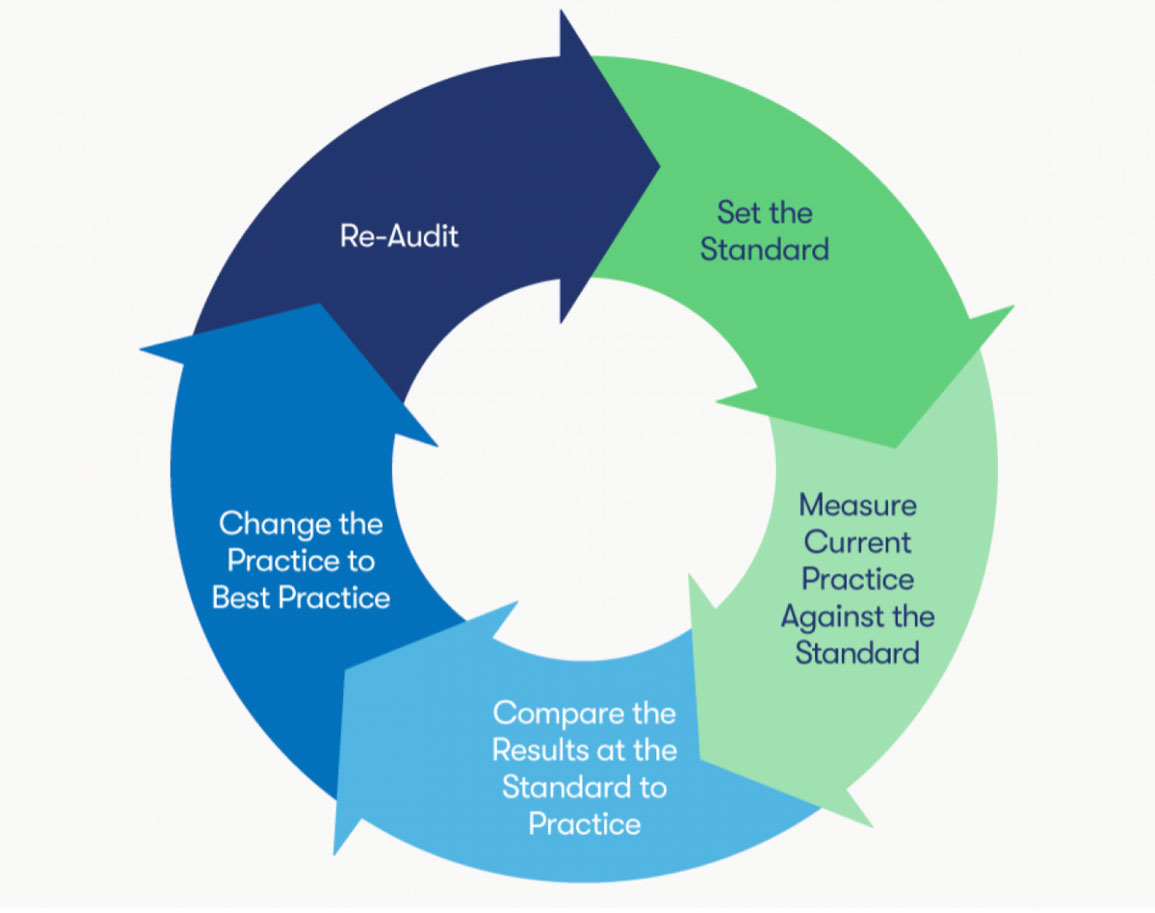
These five steps derive critical insight to help health systems apply interventions and restore revenue integrity:
1. Set the standard.
2. Measure current practice against the standard.
3. Compare the results at the standard to practice.
4. Change the practice to best practice.
5. Re-audit.
 Download
Download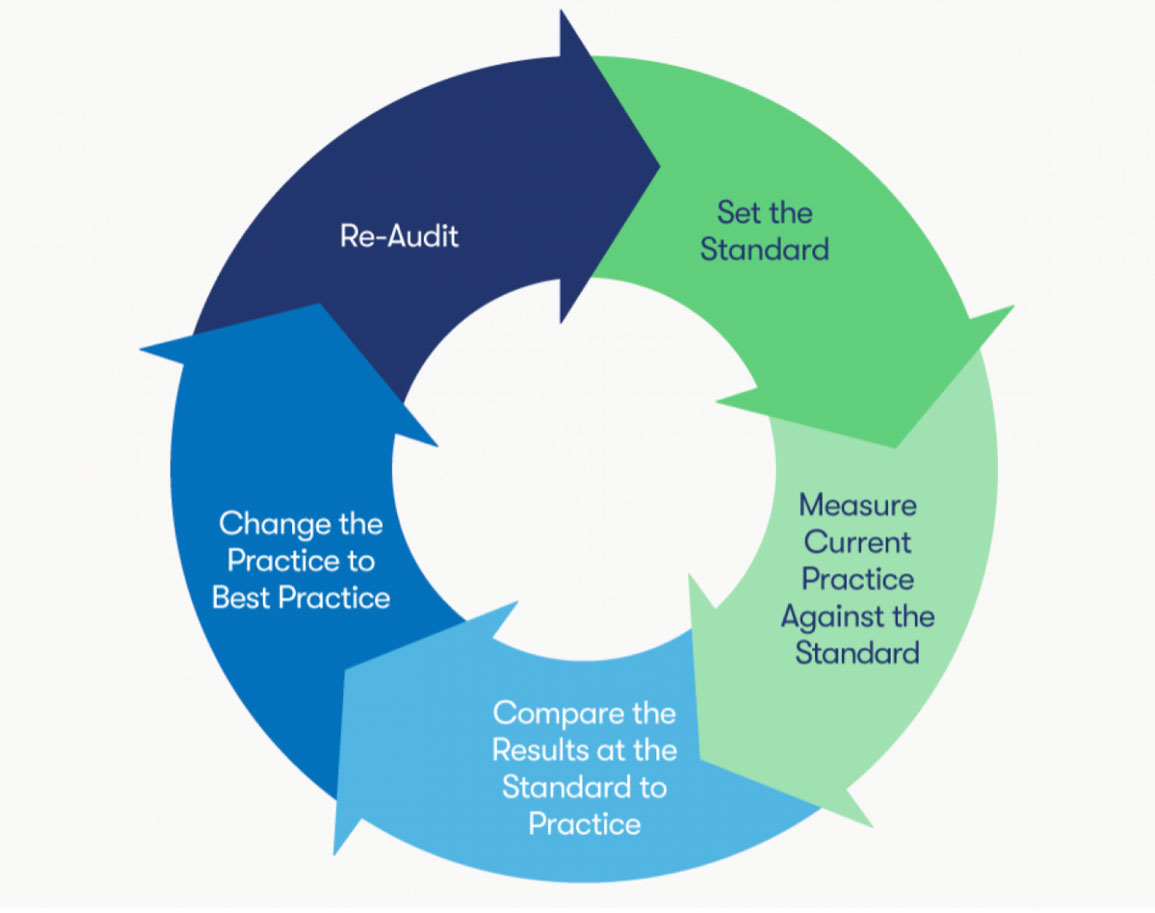
A health system’s financial well-being hinges on its ability to generate revenue through effective charge capture—the process of charging a patient or payer, then collecting money for a service, procedure, or supply. Mastering the charge capture process is an ongoing challenge for health systems, as they also face changing reimbursement guidelines and regular updates to procedure charge codes that cause lagging reimbursements and lost revenue.
The charge capture process reaches every aspect of a health system, from admitting a patient to performing surgery, yet many healthcare organizations fail to ensure peak charge capture performance. One common and often overlooked method to improve charge capture is auditing.
Charge capture auditing magnifies each step of the charge capture process, allowing financial leaders to identify problem areas that cost the health system precious revenue dollars. Many health systems use charge capture software (e.g., VitalIntegrity™) to review and understand daily charge capture performance, but organizations also need the more comprehensive insight of a charge capture audit. Charge capture auditing takes a deep dive into every aspect of the charge capture process, exposing the root causes of pricey errors or suboptimal processes so financial teams can quickly resolve issues and restore revenue integrity.
Before starting the actual audit cycle, health systems must define their audit’s objective. For example, if a health system is experiencing financial losses or inconsistencies in the pharmacy, it might choose to conduct an audit on all drug purchases. Whether organizations are auditing charge capture in the emergency department or pharmacy, they will follow the same five-step audit cycle (Figure 1).
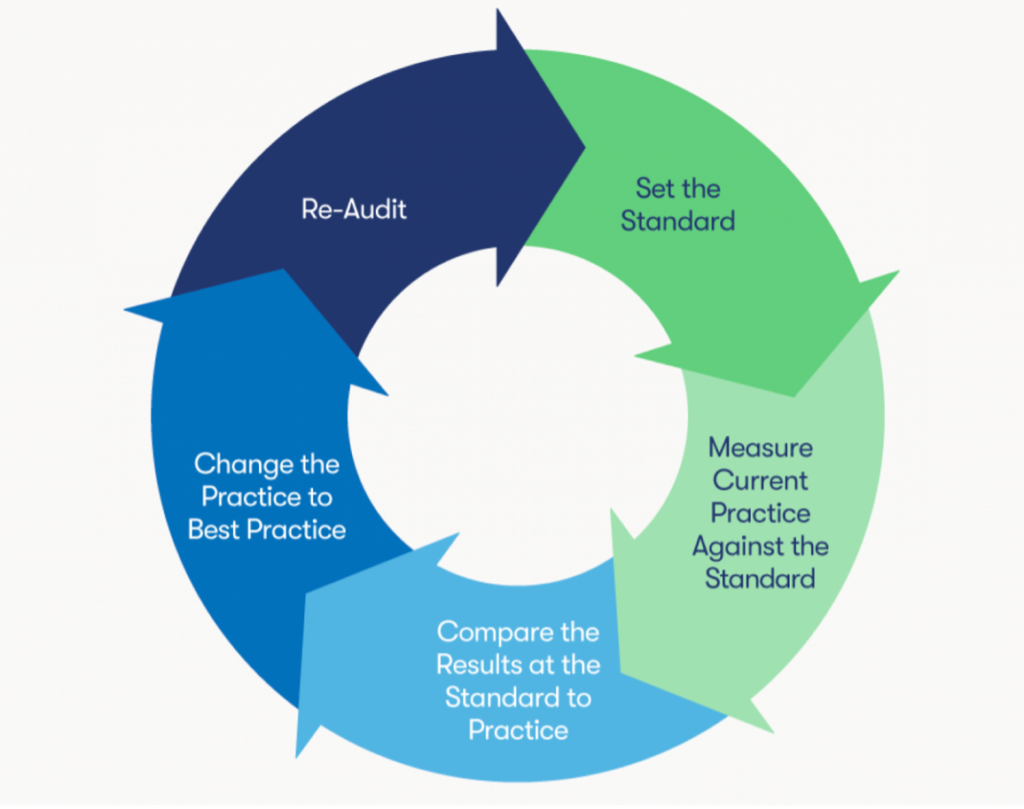
With a clear objective, systems are ready to start their audit program by following five steps:
In the first step of the auditing process, the auditing team needs to understand the standards of the process, policy, or procedure it is auditing (e.g., the health system’s CDM maintenance procedure). The auditors should use these procedure guidelines as the framework for the audit, following the step-by-step instructions to understand the expectations for the given process. The auditors will compare the audit results with these standards later in the process to identify variance in charge capture processes.
Next, the auditing team identifies and collects the data to accurately measure the current practice. The auditor must consider data quality and volume when selecting the most relevant data. For example, if a health system is conducting an audit on medical records to reduce errors, the auditor should identify the minimum number of records that would be statistically significant and accurately represent the health system’s medical record processes. By defining the data needs early in the process, health systems gain reliable insights into current medical record coding processes with the first audit and avoid unnecessary re-auditing.
By the third step, the auditor has conducted the audit and can compare the results with the data and standards from steps 1 and 2 to find discrepancies. For example, if a health system conducts an audit on mammography frequency, the auditor should randomly compare the frequency of mammograms in the mammography-eligible population with the system’s mammography standards. This ensures medical necessity—that patients don’t exceed Medicare frequency limits—which is critical for reimbursement. If the auditor finds a variance between the standard process and the current process, the health system can identify an opportunity to improve practice and reduce financial losses.
Now that the auditing team has identified discrepancies in charge capture processes, it aims to identify the root cause of the discrepancy so that leaders can resolve the errors. One method to understand the root cause is to follow the Six Sigma approach and by asking, “why?”. Below is an example of this technique:
An auditor notes a knee joint implant device (C1776) on a claim that doesn’t include a knee joint replacement procedure. First, the auditor would ask, “Why is C1776 on the claim without a procedure?” Someone from billing might reply, “Because nursing used a pick, or dropdown, list on the wrong patient.” Instead of stopping there, the auditor should continue, “Why was the wrong patient assigned a pick list for a surgery they didn’t have?” and so on until the auditor discovers the root problem.
In this scenario, the “why” questions might eventually reveal that the nurse confused two patients with the same last name because she was circulating rooms that day, signaling a failure to use the patient identification policy. In this example, the health system could reeducate the nurse and adjust and resubmit the claim for full reimbursement. This knowledge allows the health system to change charge capture practices at the root—instead of the surface—to prevent recurring problems.
After leaders have implemented process and procedural changes based on audit findings, the auditing team should conduct a re-audit to see if the changes fixed the original problems. Often, health systems implement process improvement measures to address issues but don’t realize team members have reverted to old processes, allowing the problem to resurface. Organizations can’t connect these issues back to old processes without conducting a re-audit. Re-auditing ensures the new processes are still in place and on track to improve the targeted area of the charge capture process.
As the process of getting paid for services rendered, charge capture is essential to health system survival and success. With an effective charge capture process, an organization can better manage financial risk and acquire the resources necessary to deliver care. Following the five-step audit process above allows organizations to not only deliver care to patients in need but maximize the profits for every service and procedure. Charge capture audits reveal opportunities to improve costly errors, increase charge capture accuracy, and get the revenue stream flowing again.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download this presentation highlighting the key main points.