Healthcare organizations can make the transition from a volume-focused, fee-for-service model to a value-based approach using Activity-Based Costing (ABC), a framework that tracks the true costs of delivering care. This approach supports better decision-making and patient outcomes.
 Download
Download

Editor's note: This article is based on a webinar entitled Three Keys to a Successful Margin: Charges, Costs, and Labor, presented by Bob Alexander, Cost Management, Principal, and William Malm, Vice President of Revenue Transformation, both of Health Catalyst.
As healthcare organizations grapple with rising costs and evolving payment models, achieving positive margins is more critical than ever.
The Peter G. Peterson Foundation reports that the U.S. allocates significantly more funds to fee-for-service healthcare than any other nation, nearly double the amount. Operating under a fee-for-service model incentivizes increased service volume over quality, which frequently results in excessive use of unnecessary treatments, labs, and prescriptions.
Moreover, the administrative expenses associated with managing healthcare in America are four times more than those in other affluent countries. These costs include processes such as preauthorization, claim denials, assessment of medical necessity, and dealing with multiple payers.
While the baby boomer population in the U.S. currently spends much less on long-term care than in any other country, these expanded dollars have not benefitted the American healthcare system. Indeed, the data reveals that the U.S. has the worst life expectancy, birth and infant mortality, and chronic disease management.
In an ideal world, healthcare systems consistently prioritize early intervention to prevent disease or injury, rely on proven treatment methods, avoid duplicate or unnecessary labs and testing, and eliminate less effective interventions. They would also have more streamlined technical and administrative processes to reduce indirect costs. When applied consistently and over the long term, these strategies have the potential to result in profitable margins.
These issues have long-plagued executives, but to make matters worse, the COVID-19 pandemic exacerbated challenges, and the following issues have persisted:
Healthcare leaders are also grappling with the slow adoption of value-based care or fully capitated services. In contrast, many other countries' healthcare systems operate on capitation models, where providers are paid a specific amount for a valued outcome.

In light of these issues, the U.S. healthcare system should focus on managing expenses and controlling costs since fees and reimbursements are hard to change.
Medical errors, for example, significantly impact profit margins and patient outcomes. Research indicates that these errors account for roughly $20 billion in annual costs1 in the U.S.
A possible contributor to medical errors includes surgical mistakes, diagnostic failures, medication mishaps, equipment malfunctions, technology and system breakdowns, accidental falls, and a lack of hospital staff. Hospitals frequently downsize nursing staff to cut costs. This talent shortage contributes to heavier patient workloads linked to increased mortality rates.
"Now nurses are being sued and have criminal convictions for medical errors. More and more people are leaving the industry; they no longer want to accept liability.2" — William Malm, Vice President of Revenue Transformation, Health Catalyst.
Hospitals and physician practices seek ways to work smarter and more efficiently with fewer medical errors. They also look to increase the bandwidth of their staff using modern technologies, such as AI, and provide more preventive care to reduce hospitalizations.
To achieve these aims, healthcare organizations must transition from volume to value, improving margins, boosting quality, and eliminating waste.
A Value Creation Framework, a process improvement methodology, addresses all three areas by implementing best practices, employing data and analytics, and adopting a new culture, leading to sustained improvement.
The Value Creation Framework involves the following initial steps:

Data and analytics play a critical role in this process improvement methodology.
Yet, most hospital data goes unused or misused. Health systems must capture the correct and relevant data about their processes to employ the Value Creation Framework and ensure that this data is accessible broadly. Next, end users must be able to generate valuable insights from the data and promote more informed decisions.
Inconsistent data can lead to revenue leaks that drain resources. For example, capturing charge master data has become a critical priority as charge capture leakage in healthcare hovers around 1 percent nationally.
Despite improvements thanks to automation, charge capture processes still occur within silos, continuing the charge loss phenomenon that degrades hospital margins. Failing to secure potential reimbursements leads to a decline in revenue, while incurred expenses diminish profit margins related to costs and charges.
Consequently, healthcare organizations must proactively oversee charges before claim submission and prevent the complications linked with charge leakage and delayed billing. Achieving this necessitates moving past simple charge reconciliation toward a more comprehensive, data-oriented approach that leverages appropriate technologies, especially given that many health systems may not have sufficient personnel to manage these responsibilities.
An example of this is an AI tool employing rules-based logic to analyze all daily charges comprehensively. When a trigger appears within the charges—such as a procedure, service, supply, or medication—the system searches for a corresponding target. If the target is found, the rule remains inactive.
Conversely, the charge gets flagged for manual examination if the target is missing. This integration of technology enables a complete review of all charges, which was not achievable before when health systems had to be more selective in conducting audits.
The issue of charge capture management is just one example of why healthcare systems need a much more effective and comprehensive cost management system.
The Ratio of Cost to Charges (RCC) and Relative Value Units (RVU) have long been used in healthcare to estimate costs. However, both methods have significant limitations when applied in medical settings:
Without a reliable understanding of what it costs to provide patient care, hospitals and health systems continue to struggle to agree on basic information about their services, such as which are most profitable.
“Cost management methods such as Relative Value Units (RVUs) or Ratio of Cost to Charges (RCC) were necessary in the 1980s, 90s, and 2000s. Methods like Time-Driven Activity-Based Costing (TDABC) are very applicable in a manufacturing setting where you have a very predictable assembly line or process that your product goes through to be produced. But in healthcare, you have a chaotic situation where it’s hard to predict (with time estimates) what will happen in your hospital or with patients each day—will their conditions worsen or improve? Without a reliable understanding of what it costs to provide care to patients, hospitals and providers struggle to answer basic questions like ‘what services are most profitable?’, ‘what should we stop doing?’ and ‘does everyone agree on the answers?’ With better data, you can start to answer these questions with more objective truths rather than relying on subjective opinions.” — Bob Alexander, Cost Management, Principal, Health Catalyst.
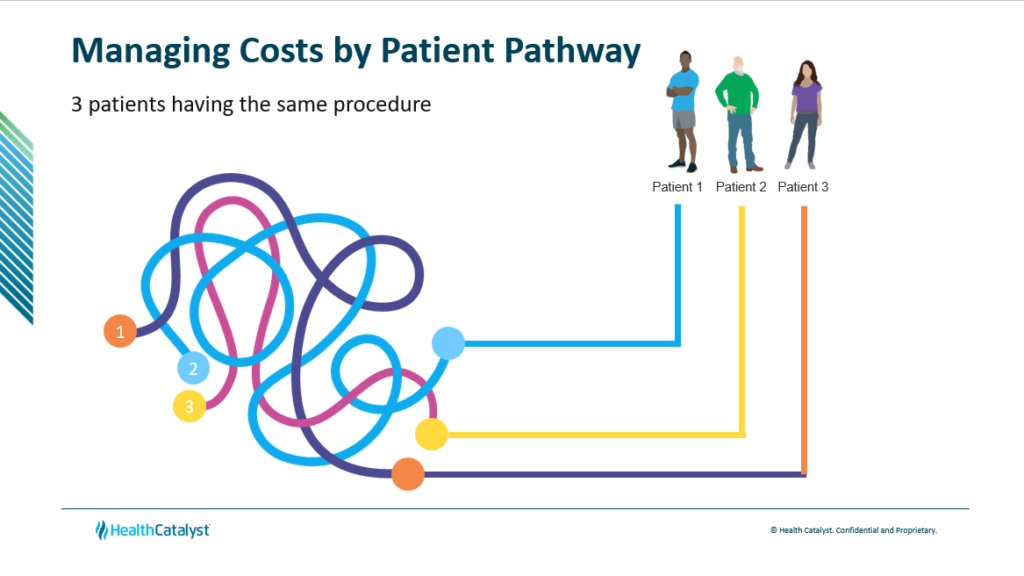
Activity-Based Costing (ABC) offers a more accurate and comprehensive approach to understanding the true costs of service delivery by tracing costs to specific activities and resources used in patient care. ABC leverages detailed data, often collected through Electronic Medical Records (EMRs), allowing for precise cost assessment and allocation.
Health systems have observed the following advantages of using the ABC approach:
The ability to capture and analyze data is crucial for implementing value-based costing models. Health systems need data sets that give them the granularity and specificity required to make decisions, but that can also scale and view these data sets at a high level.
Health Catalyst's PowerCosting™ uses detailed data from EMRs to track clinical costs accurately. The software allows for real-time tracking, which will enable organizations to:
Advanced technologies allow providers and executives to examine any procedure or group of procedures across providers and see payment variability to determine which procedures support the bottom line. For instance, they can see whether one provider's approach, such as their vendor selection, leads to profit and if another provider's approach leads to loss.
"We want to show providers data so they can make the best decisions at the point of care. We can inform the providers and the administrators, get everyone on the same page about how we're tracking procedures and supply costs, and learn which methods are viable."— Bob Alexander, Cost Management, Principal, Health Catalyst.
The transition from volume to value in healthcare requires more than just a change in payment models; it demands a fundamental shift in how costs are understood and managed.
By leveraging detailed information from EMRs and focusing on the actual costs of delivering care, health systems can make data-driven decisions, reduce waste, and optimize the use of resources, leading to improved margins and a more manageable shift to value-based care.

Would you like to learn more about this topic? Here are some articles we suggest:
PowerCosting™ Improves Strategic Decision-Making, Increasing Revenue by $10M
Charge Capture Improvements Increase Revenue by $552K